If you have been wondering whether or not a ketogenic diet can help chronic fatigue then the short answer is: Yes and, it depends.
If you would like to understand whether or not a ketogenic diet may be appropriate for you and where you fit into the nuance of it all, then keep reading.
I’ll also be covering:
- What is a ketogenic diet?
- How could it be supportive for chronic fatigue?
- How to implement and transition into a ketogenic diet if you have fatigue or a chronic illness
- Top tips to maximise the benefits of your ketogenic diet
- How to avoid the “keto flu”
Let’s start with the basics…
What is a ketogenic diet?
The ketogenic diet is a high fat, low carbohydrate and moderate protein diet intended to shift the body away from burning sugar as a primary fuel source and allow the body to produce ketones which convert to the body’s energy currency, ATP.
In the absence of sugar as a fuel, the liver creates ketones, in the form of acetoacetate and beta-hydroxybutyrate, from fat. It may be quite normal to enter a natural state of ketosis in the gap between your evening meal and your first meal of the day and this is reflected in a blood ketone level of 0.5 mmol/L or greater.
The process of switching to using ketones for energy is known as “nutritional ketosis”. The ketogenic diet is a means to achieve nutritional ketosis, which allows for the body to remain in ketosis without fasting or starvation. i.e. after an overnight fast, you can remain in ketosis for the rest of the day based on your food choices.
Nutritional ketosis has been found to improve metabolic and inflammatory markers, including lipids, HbA1c, high-sensitivity CRP, fasting insulin and glucose levels, and aid in weight management. Research suggests that it may be helpful in the following conditions:
- Obesity
- Metabolic Syndrome
- Type 2 Diabetes
- PCOS
- Neurodegenerative Disease and Pain Syndromes (more on this later)
- Traumatic Brain Injury and Epilepsy
- Skin Conditions such as acne
- Some forms of Cancer
- Digestive Disorders such as IBS and GERD
But What About Fatigue?
Fatigue is the consequence of a reduced capacity to produce the body’s energy currency, adenosine triphosphate abbreviated as ATP. ATP is produced through a series of biochemical steps which include:
- Sugar burning or glycolysis; this step produces 2 ATP
- Fat Burning also known as “Beta-Oxidation” which produces 30-38 ATP
Therefore, provided these systems are working well, we have far greater potential to make ATP when we are efficient at using fat as a fuel source.
A recent research paper has suggested that people with ME/CFS may have altered metabolic pathways when compared to healthy controls. Some people with ME/CFS may have increased rates of glucose metabolism but disturbed mitochondrial metabolism. In other words, they burn sugar well but don’t burn fat so well.
One of these altered metabolic pathways is known as the “Warburg Effect” which refers to a mode of energy production where glucose is preferentially used to make lactate. A clue that someone may be experiencing the Warburg Effect is muscles that ache all the time, especially with exercise and physical exertion and they may show high levels of lactic acid in an organic acid urine test.
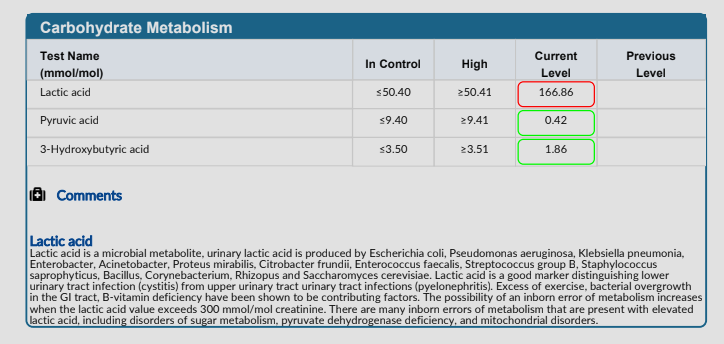
The ketogenic diet may be helpful in the case of high lactate levels because the body can produce energy from ketones and bypass glycolysis which generates high blood lactate.
This is one of the mechanisms by which the ketogenic diet can be helpful for fatigue, but there are others, the most important one to highlight is how it may be supportive in blood sugar balance and the anti-inflammatory benefits for those experiencing neuroinflammation.
Blood Sugar and Fatigue
Recovering from Chronic Illness and Chronic Fatigue requires physiological stability. One of the ways we can stabilise the body physiologically is by stabilising blood sugar. Practically what this means is ensuring that blood sugar fluctuates within a narrow range each day.
When blood glucose and/or insulin is high there is poor brain glucose penetration and as a consequence, low brain energy. The resultant effect is the conversion of stem cells into immune or inflammatory cells, which can drive brain inflammation.
This may be associated with symptoms such as cognitive fatigue, brain fog and headaches.
Additionally, insulin can increase histamine levels which, if you are someone who experiences symptoms of histamine intolerance or Mast Cell Activation Syndrome (MCAS), can turn the volume up on symptoms.
Finally, high levels of insulin uncouple mitochondria which prevents the generation of ATP (your energy currency) along the electron transport chain, contributing to fatigue.
Low blood sugar isn’t better. When blood sugar drops too low it increases free radical production. Free radical damage mitochondria and this impacts ATP production.
Additionally, low blood sugar increases sympathetic tone of the autonomic nervous system (ANS) which can lead to feelings of being “tired but wired”.
Whether your blood sugar is too high, too low or swinging between the two, you definitely want to stabilise it if you want to improve your fatigue and increase your energy.
I have an entire blog which goes into the in’s and out’s of stabilising blood glucose in more detail. Sometimes a ketogenic diet (and intermittent fasting) is required to stabilise blood glucose, improve metabolic flexibility, reduce inflammation and in doing so, increase ATP production, energy and healing.
Who is a ketogenic diet NOT appropriate for?
By now you are probably getting an understanding of how the ketogenic diet can be supportive in chronic fatigue and chronic illness. However, it is not necessarily suited or appropriate for everyone. You may want to seek support from an appropriately trained practitioner, proceed with caution or avoid it if you are:
- Struggle with low blood sugar and hypoglycemia; the first goal in this instance would be to stabilise blood sugar with frequent and well balanced meals before you attempt to achieve ketosis or use any fasting protocols.
- Pregnant or Breastfeeding
- Suffer from Gallbladder Disease of if you’ve had your Gallbladder removed
- Suffer from Kidney Disease or Kidney Stones
- You are going through or have gone through a very stressful time resulting in dysfunction of your HPA-axis – this can be determined with testing through a Functional Medicine Practitioner if necessary
- Athletes may need to tailor their dietary requirements to their sport
How do you know a ketogenic diet is right for you?
Even if you do not have any of the contraindications listed above, how do you know a ketogenic diet would help you move the needle in your chronic fatigue recovery?
What I will share is that we are seeing more and more clients who benefit from a ketogenic diet and although we do not advocate for a “one size fits all approach” we are recommending a ketogenic diet more and more.
In practice we guide clients towards a ketogenic diet on a case by case basis. This usually starts with a review of their bloodwork blood sugar monitoring to make an assessment of their glucose stability – you can read more about this here.
Our preference is to focus on stability first which means:
- Stabilising meal times: is the person eating 3 regular meals per day or are they skipping meals and eating erratically. If the answer is the latter, we want to stabilise meal times before we move into making dietary changes.
- Stabilising meal balance: if the person doesn’t have a good balance of protein, fat and fibre with each meal, this would be the initial goal before titrating carbohydrate down and fat up.
- Stable sleep routine: poor sleep impacts blood sugar and stress hormones and blood sugar and stress hormones impact sleep. It is a bit of a chicken and egg situation but we may want to work towards good sleep routines and supporting sleep before transitioning to a ketogenic diet.
- Stable movement routine: an exercise or movement routine – within the individuals capacity – is essential for energy recovery. This means doing the same thing each day preferably at the same time.
- Nervous system stability: if the individual is in a high state of stress we want to make sure that they have a toolbox to support their nervous system before making dietary changes that could be overwhelming.
With these things in place we could then consider transitioning to a ketogenic diet.
How to Transition?
The assumption at this point in time is that you have some foundations in place. Here is a checklist you can use as a guide:
- I am eating 3 regular meals per day
- My meals are balanced with protein, fats, fibre and carbohydrate
- I am eating adequate calories to meet my needs
- I have a sleep routine (even if I don’t always sleep as well as I would like)
- I have a movement routine that is within my capacity
- I feel mentally ready to make dietary change
- This feels like the next important step in my journey
- I have no contraindications for following a ketogenic diet
Assuming that all of the above is in place the next steps can be very simple or we can get a little more technical.
Here is the simple version
- Titrate your carbohydrate down usually in the order of:
- Removing any refined sugars and flours
- Removing fruits (sometimes we keep a small amount of berries if tolerated)
- Removing grains
- Removing root vegetables
- Titrate your fats upwards
- Ensure adequate protein consumption (0.75g/1g per pound of ideal body weight)
- Maintain adequate calories to meet your needs
Implementation (for those who are more detail oriented)
The ketogenic diet is based on a macronutrients (protein, carbohydrate and fat) intake which may look as follows:
- 60 to 75 percent of calories from fat
- 15 to 30 percent of calories from protein
- 5 to 10 percent of calories from carbohydrates
In our opinion a ketogenic diet is ANY diet that allows you to achieve nutritional ketosis which is blood ketone levels of 0.5mmol/L or more. Therefore we feel the percentages are less relevant than what is actually happening in your body.
You can assess blood ketones using a Keto Mojo [use the link for 15% off the UK and EU Stores] which is a finger prick device that will allow you to measure your blood glucose and blood ketones. A blood ketone monitor will be superior to breath testing and urine strips.
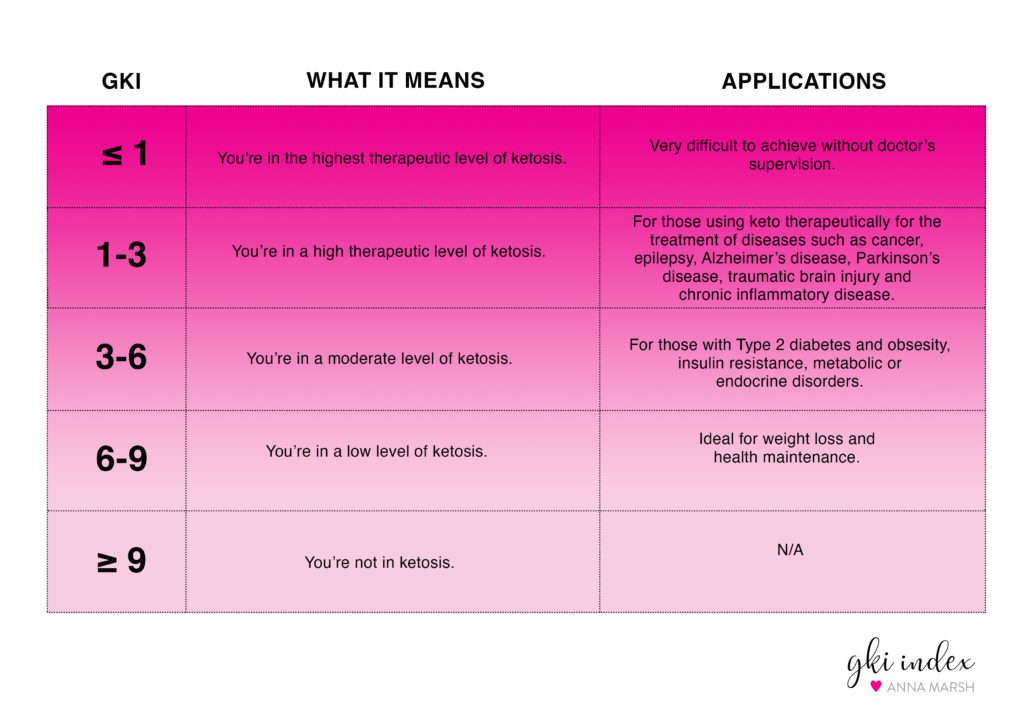
Keto Mojo also promotes a concept called GKI or Glucose Ketone Index. This is the ratio of glucose to ketones in your bloodstream calculated by dividing your glucose measurement in mmol/L by ketones in mmol/L.
For example, if your blood glucose was 5 mmol/L and your ketones were 1mmol/L then your GKI score would be 5. They propose certain health benefits based on the level of ketosis achieved. See diagram below:
Should you count calories?
Although many experts advise not to count calories while following a ketogenic approach. Calorie counting is not for everyone but we feel that having a rough guide about how much you should eat is helpful. This prevents under-eating and fatigue, lethargy, cravings and hormonal imbalances which can be symptomatic of inadequate fueling. It also guards against overconsumption which can be counter- productive to health benefits.
There are various calorie calculators online, such as this one. Keep in mind that this is just an estimate and we all have our unique needs and your actual requirements may fall a couple of hundred calories over or under these guidelines.
You can use an app, such as My Fitness Pal (MFP) to track my total calories and carbohydrates, fats, proteins, fibre and grams of sugar. We often advise tracking your intake before you make any changes so that you can see what your current baseline looks like and then take intention steps to aid the transition to where you want to be.
You don’t have to track food forever, but a few weeks may set you up nicely until you feel confident with your food choices.
Here is how Anna transitioned when she followed a ketogenic diet
I didn’t immediately throw myself into a ketogenic diet. My baseline carbohydrate intake was already fairly low at about 100-120g per day. I began by lowering my carbohydrate to around 70g-80g per day. At the time I used blood sugar monitoring before eating, 1 hour after eating and 2 hours after eating.
Over time I reduced my carbohydrate intake to around 50g per day, using My Fitness Pal to monitor my intake. This 50g was inclusive of vegetable fibres. My fibre intake was often between 25g and 35g leaving a net carbohydrate intake of around 15g-25g per day.
At the time, due to gut dysfunction, I followed a lower protein diet, around 0.5g of protein per pound of ideal body weight, which meant my protein intake was around 70g per day. If protein is poorly digested there is an increased potential for it to contribute to oxidative stress which drives damage and inflammation. As my digestion healed I increased my protein intake to the recommended amount of 0.75g-1g per pound of ideal body weight, which was around 120g-140g per day.
My fat intake made up the rest of my calories, which you can calculate using a total daily energy expenditure (TDEE) calculator. This meant that I would consume around 130g-150g of fats per day. These mostly came from butter, coconut products (yoghurt, oil, milk), avocado, olive oil, oily fish, nut butters (especially macadamia nut butter as a treat), 85% dark chocolate and animal proteins.
Top Tip:
Remember, once you have completed your transition you want to adhere to it for 3 or 4 weeks to give yourself time to fully feel the benefits. You can confirm you have actually achieved ketosis by using a blood ketone monitor. You are fully fat adapted when you have negative urine ketones and positive blood ketones.
What Can You Eat on a Ketogenic Diet?
The ketogenic diet is a high fat, low carbohydrate and moderate protein diet. It may often be associated with eggs, bacon, butter, cheese and cream however, if you are implementing a ketogenic diet for health benefits and recovering from a chronic illness or chronic fatigue, you’ll want to approach it from a perspective which allows you to maximise it’s healing potential and minimise inflammatory foods.
Proteins
Unless otherwise required, aim to consume 0.75g-1g of protein per pound of ideal body weight. Consume proteins from:
- Sustainably sourced oily fish, white fish and seafood
- Meat; Beef, Pork, Lamb – ideally grass fed and regeneratively farmed
- Poultry; chicken, turkey, duck etc.
- Venison
- Eggs
- Protein powders without sweeteners or added carbohydrates e.g. whey, beef, pea
- Edamame Beans (if soy is tolerated)
- Nuts and Seeds
You can allow for some dairy such as cheese and full fat greek yoghurt but a lower dairy diet or no dairy diet may be beneficial in some cases.
Fats
Fats should make up the bulk of your calorie intake. Choose from:
- Oily Fish
- Fatty cuts of meat and poultry – ideally grass fed and regeneratively farmed
- Eggs
- Coconut products; coconut milk, coconut oil, coconut yoghurt, coconut chips, unsweetened
- Nuts and nut butters
- Seeds and cold pressed seed oils
- Olives, olive oil
- Avocado
- Dark chocolate (85%+) in moderation
- Butter or ghee
You can allow for some dairy in addition to butter in the form of cheese and full fat greek yoghurt but a lower dairy diet or no dairy diet may be beneficial in some cases.
Fibre
Although you are following a low carbohydrate diet, my encouragement is to emphasise a variety of colourful vegetables, herbs and spices in your diet so that you receive the antioxidants benefits. Focus on:
- Leafy greens
- Brassicas
- Onions and garlic
- Peppers
- Tomatoes
- Fresh herbs
- Spices
Avoid:
- Potato
- Sweet potatoes
- Grains
- Pumpkin and Squash
- Beetroot and carrot (small amounts may still allow for ketosis in some cases)
- All fruits (berries may still allow for ketosis in some bases)
- All refined sugars (sweeteners like stevia or monk fruit extract may be allowed)
Polyphenols are a group of plant-based compounds that have been reported to be particularly beneficial in combating oxidative stress. They are neuroprotective and have potential to suppress neuroinflammation and promote memory, learning, and cognitive function. As you engage with a ketogenic diet you may want to focus on the following. Berries in small amounts may still allow for ketosis in some individuals – you will need to test your blood ketone levels and assess if they are appropriate for you.
The most abundant sources of polyphenols that may be ketogenic diet compliant are, in order of abundance:
- black elderberry
- black chokeberry
- blackcurrant
- highbush blueberry
- globe artichoke heads
- filter coffee
- lowbush blueberry
- sweet cherry
- strawberry
- blackberry
- red raspberry
- flaxseed meal
- dark chocolate
- chestnut
- black tea
- green tea
- hazelnut
- cacao powder
- black olive
- spinach
- pecan nut
- prune
- soy tempeh
- soy tofu
- green olive
- red onion
- roasted soy bean
- shallot
- red chicory
- broccoli
Side Effects
When you already feel unwell with fatigue there can be a lot of resistance against doing something that may make you feel worse in the short term.
And it is true, there can be a period of transition as one moves from a higher or “normal” carbohydrate diet to a ketogenic diet. As insulin levels begin to fall, this can be associated with constipation, headache, halitosis (bad breath), muscle cramps, diarrhoea, general weakness, and skin rashes.
These effects can last between 1 to 4 days and sometimes longer depending on the degree of adaptation required for each individual. Gastrointestinal symptoms can be associated with maldigestion of fat due to increased intake, poor liver and gallbladder function (We see poor fat digestion in mant of the stool tests we run with clients so this is a real concern) or a non-intentional reduction of fibre due to a change in food choices.
With any dietary change the digestive system may need a few days to catch up. If unwanted side effects still persist, digestive support in the form of apple cider vinegar, enzymes, tudca, lipase or bile acids can be helpful. It is also important to embrace eating plenty of colourful plant-based foods for adequate fibre.
Fasting or even a low carbohydrate diet lends itself to lower circulating levels of insulin, the hormone that rises after a meal to manage sugars entering the bloodstream. Electrolytes are minerals that have an electric charge. These include calcium, potassium, magnesium, chloride, and sodium, the levels of which are regulated by the kidneys.
As insulin levels reduce this can cause the kidneys to excrete electrolytes, specifically sodium, and water. This can account for rapid weight loss experienced in the first few days of initiating such a diet.
This is one of the beneficial mechanisms by which blood sugar and insulin management can be healthful for low blood pressure. However, loss of electrolytes can also be associated with some of the symptoms of what is colloquially known as the “keto flu”. These symptoms may include:
- Headaches
- Nausea
- Drowsiness
- Fatigue and low energy
Therefore as you enter into a state of ketosis it is important to keep sodium levels topped up. You can do this with food or by topping up with electrolytes.
- Olives
- Biltong
- Cured meats
- Salt your food
- Add a pinch of sea salt to drinking water.
- High quality stock cubes mixed with hot water as a “cuppa soup” – add more salt if required
- Homemade bone broth – add extra salt if required
Or consume electrolytes, these are some of my favourites:
These electrolytes are available on amazon.
Alternatively you can take LMNT if you are US based or RePowr if what we recommend for our UK clients. You can use the link for 10% off. Both taste great and comes in convenient portion sized packets.
Supporting Sleep As You Transition
Blood sugar lows during the night can drive up stress hormones causing poor sleep. The same can be true for low ketones during the night. Therefore a tablespoon of MCT oil before bed may help with a restful night’s sleep.
What About Fasting?
Fasting can complement a ketogenic diet and it can also be great for supporting chronic illness and chronic fatigue. We recommend fasting to clients on a case by case basis because, as with the ketogenic diet, there can be nuance when it comes to appropriateness. Therefore, fasting requires its own blog.
Fasting is best implemented when one is full fat adapted. This is determined by negative urine ketones but positive blood ketones. When you first transition to a ketogenic diet you can expect that ketones spill over into the urine. As the body adapts to use them as fuel, lower amounts will be seen in the urine.
A safe and easy intervention that is appropriate for most people is to ensure a daily overnight fast of 12 hours which can be extended to 14 or 16 hours if that feels good to the individual.
Within the eating window, I recommend reducing meal frequency. This means limiting food intake to 3 meals per day or possibly 2 meals or 2 meals and 1 snack if the window is shorter e.g. 8 hour feeding window.
You’re All Set!
By now you should be a little more clear if this is the best next step for you and where to get started. If you want more help on your fatigue and / or chronic illness recovery journey, learn how to balance blood sugar, implement a ketogenic diet and fast, take our blood sugar mini course for just £49!