The Importance of Balanced Blood Sugar in Fatigue Recovery
Although healing from a Chronic Illness, such a Chronic Fatigue Syndrome (CFS/ME) can be complex, basic principles will always form the foundations of a successful recovery journey. Sometimes the basics are almost too simple and can easily get overlooked in our search for answers or looking for more complex root causes.
Blood Sugar Balance is one of the pillars of the “Foundational Five Methodology“, the other four pillars being nervous system, sleep, pacing and managing inflammation (you can take the FREE Quiz, to identifty which are most important for you). Blood sugar should fluctuate within a narrow range each day and there should be no excessive highs or excessive lows.
Both high and low blood sugar negatively impact energy production. High blood sugar means that glucose isn’t getting into the cells where it can be converted to energy. Low blood sugar increases cortisol levels and sympathetic activation of the nervous system, which is disruptive to creating a healing state. In the early stages of fatigue recovery we want to create as much stability as possible to allow for healing.
Therefore, it is difficult to recover and feel well, without stable blood sugar. I recommend that everyone does some blood sugar monitoring at some point in their journey – sooner rather than later in my opinion – even if all they do is rule it out as a problem.
Carbohydrates In Your Body
When we eat a meal, carbohydrates, in whatever form, are digested and broken down into glucose in the gastrointestinal tract. From here they are absorbed into the bloodstream. From the bloodstream they can be used immediately for energy or stored in tissues like muscle or liver for future use.
The ability to use glucose (sugar) as fuel is dependent on glucose (sugar) getting into the cells of the body. All cells in the body use glucose. Therefore, these cells must have insulin receptors and the body must produce insulin, from the pancreas, to facilitate the transport of glucose into the cell.
A healthy individual eating a balanced diet will produce adequate amounts of insulin to carry glucose into the cells and store glucose appropriately. While this is happening their body is maintaining a glucose balance between approximately 4mmol/L and 6.1 mmol/L.
Let’s say this person ate a meal that was very high in carbohydrate like a big bowl of pasta or a giant piece of cake. A lot of sugar may enter their bloodstream and then one of three things may happen.
- Their body may respond with an insulin surge to take the sugar out of the blood stream to maintain homeostasis.
- The same as above but their blood sugar may crash too low a couple of hours later.
- Their body may respond with an insulin surge, but it might not be enough to deal with all the glucose, resulting in elevated blood sugar.
- Their body may respond with an insulin surge but their cells are not sensitive enough to the insulin which blocks the glucose from getting into the cells, resulting in elevated blood sugar.
Number 1 is the ideal scenario. Numbers 2, 3 and 4 are examples of dysfunctional blood sugar control and this can have the following consequences;
When blood sugar and/or insulin is high there is poor brain glucose penetration and as a consequence, low brain energy. The resultant effect is the conversion of stem cells into immune or inflammatory cells, which can drive brain inflammation. This may be associated with symptoms such as cognitive fatigue, brain fog and headaches.
Additionally, insulin can increase histamine levels which, if you are someone who experiences symptoms of Histamine Intolerance or Mast Cell Activation Syndrome (MCAS), can turn the volume up on symptoms.
Finally, high levels of insulin uncouple mitochondria which prevents the generation of ATP (your energy currency) along the electron transport chain, contributing to fatigue.
These are all examples of mechanisms by which high blood sugar and high insulin levels may contribute to the total picture of fatigue. But what about low blood sugar?
Low Blood Sugar
If high blood sugar is bad, low blood sugar isn’t better. Blood sugar may drop low due to:
- Under-eating
- Over-exercising
- High stress
- Imbalanced meals i.e. too much carbohydrate and not enough protein, fat and fibre
- Loss of adrenal resiliency (which is the ability of the adrenal glands to step in to regulate blood sugar in times of low glucose availability)
Sometimes blood sugar can swing between high and low, for example, it may go initially high after a meal and then crash 2-3 hours later. When blood sugar drops too low it increases free radical production. Free radicals damage mitochondria and this impacts ATP production.
Additionally, low blood sugar increases sympathetic tone of the autonomic nervous system (ANS) which can lead to feelings of being “tired but wired”.
Whether your blood sugar is too high, too low or swinging between the two, you definitely want to stabilise it if you want to improve your fatigue and increase your energy.
How do you know if this is a problem for you?
A quick and easy way to understand if blood sugar imbalances are impacting your energy is to look for energy changes around meal times.
Low energy prior to eating with a “pick me up” after a meal, can be a sign of hypoglycemia. Sugar cravings and relying on coffee in the afternoons after having lunch could be another sign.
Low energy after a meal can be a sign of high blood sugar or high insulin. Energy crashes after eating can also be due to food sensitivities or high histamine load so you may want to rule this out too if you feel your blood sugar is on point.
But my doctors says my blood sugar is “normal”?
This diagram shows the progression of the onset of type 2 diabetes. Changes in fasting blood sugar are one of the diagnostic criteria for type 2 diabetes. You can see that changes in fasting sugar levels (the black line) begin to occur at point “0” on the graph which represents time of diagnosis.
However, insulin secretion (the green) line is increasing from -10 years. Beta-cells are the cells in the pancreas that produce insulin. They are represented by the green line on the graph. The function of these cells begins to decline from -10 years. The message here is that type 2 diabetes is developing as early as 10 years prior to diagnosis.
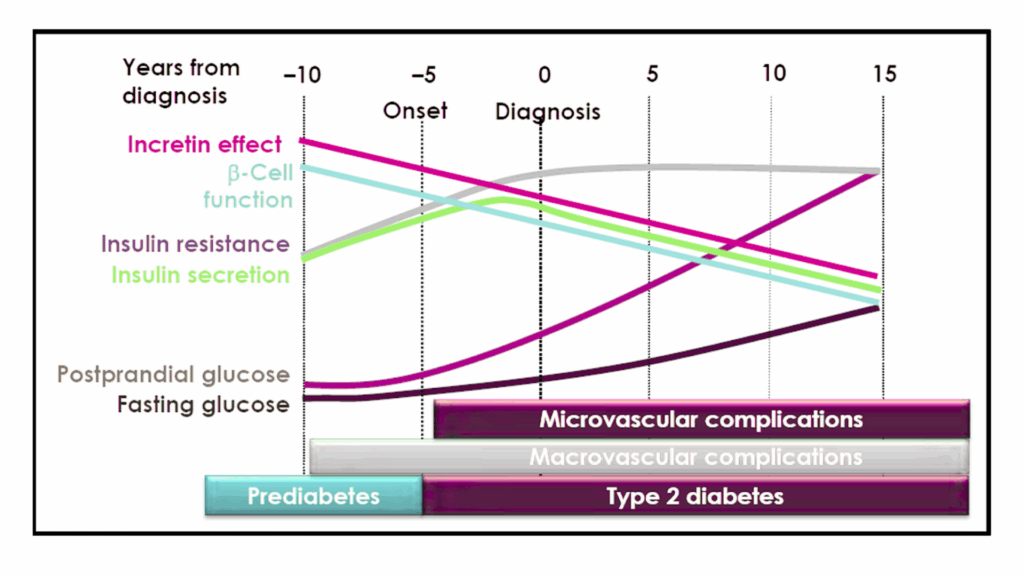
To summarise, as blood sugar balance begins to change, this is what we will see:
- Stage 1: Increase in insulin after meals
- Stage 2: Increase in glucose after meals
- Stage 3: Increase in fasted insulin
- Stage 4: Increase in fasted glucose (point of diagnosis)
This means we can intervene earlier and catch imbalance before it becomes disease if we monitor glucose after meals.
This is something I ask all my clients to do, even if all we find is that everything is normal. It is important to rule it out. It is something that you can do, exactly how to be discussed shortly.
What about HB1AC?
Haemoglobin A1c (Hb1AC) measures glucose attached to haemoglobin and it is an indicator of average glucose across a 3 month period of time. It is assumed that if your Hb1AC is below 40 mmol/mol that you are healthy.
However if your blood glucose is swinging between high and low throughout the day, the two will cancel each other out and the average will look normal. I still ask my clients to monitor their blood glucose even if their Hb1AC looks perfectly fine.
Other Clues
Insulin: You can ask your doctor for a 2 hour postprandial insulin level or fasted insulin level, however remember that fasted insulin may only change further along the progress towards type 2 diabetes. Postprandial insulin may be difficult to get.
Triglycerides: elevated triglycerides can be a signal for insulin resistance. I like to see my clients with TGs under 1.7 mmol/L.
TG/HDL: The ratio of triglycerides to High Density Lipoprotein (HDL) Cholesterol can also be indicative of insulin resistance. Ideally you want this ratio to sit below 3.
Self Glucose Monitoring
Self glucose monitoring is an easy way you can assess yourself meal by meal. It will allow you to identify trends in your blood sugar and adjust your diet to optimise your glucose balance.
How do you do it?
You’ll want to use either a finger prick glucometer or a continuous glucose monitor (CGM). I initially start clients with a CGM to get a big picture overview of what might be happening for them. For ongoing monitoring, a fingerprick monitor can be financially more sustainable. CGMs have their limitations and, at times, can produce unreliable data. If you do decide to use a CGM I suggest that you also purchase a finger prick monitor so that you can double check the data.
I personally use a keto mojo [use the link for 15% off at UK and EU Stores] which is a bit more of an investment but I trust the accuracy and accuracy is important when you are wanting to keep your glucose within narrow margins. If you are interested in blood ketones I would highly recommend getting one.
Once you have your device of choice, here are some readings you may want to track:
- Waking BS: ideally <5.5 mmol/L but may be higher in times of stress or poor sleep
- Pre-meal BS: ideally below <5.5 mmol/L
- 45 minute post meal BS: ideally <6.1 mmol/L
- 60 minute post meal BS: ideally <6.1 mmol/L
- 2 hour post meal BS: ideally below <5.5 mmol/L
- Before bed: ideally below <5.5 mmol/L
- Any other times you may be curious: ideally between 4 mmol/L and 5.5 mmol/L unless you are within the first two hours of eating
It may go without saying but once you have eaten your meal you will want to avoid eating or drinking anything that would increase your blood sugar until after you have taken your measurements.
What does it mean if your glucose is high?
Dysfunctional glucose metabolism would be considered if:
- Your glucose peak, which is around 45 minutes to 1 hour after a meal, is higher than 6.1 mmol/L
- Your glucose does not return to a healthy level (e.g. below 5.5 mmol/L) within two hours of eating
If this is the case you then need to play detective and work out why. The best place to start would be your diet. This might mean:
- Improving the quality of carbohydrates in your diet: swop more refined and processed carbohydrates (e.g. bread, pasta, white rice) for more whole carbohydrates (brown rice, sweet potato)
- Reduce total consumption: you may need to reduce the total amount of carbohydrate you consume across the day by reducing portion size – even if you are eating quality carbohydrates, you may be eating too many
- You may need to increase protein at your meals.
- You may need to increase fats at your meals.
- You may need to increase fibre (vegetables) at your meals.
- You may want to eat the protein, fat and fibre first and eat the carbohydrate portion last.
Personal Story
Blood sugar imbalances were a blindspot in my fatigue recovery and fortunately very early on I worked with a well trained practitioner who picked up on it straight away. I did the blood sugar monitoring – in fact 4 years later I still check in, I have my keto mojo on my desk as I type this – and found that I had to strictly follow a ketogenic diet to bring my blood sugar into the correct balance.
Not everyone may need to go to this extreme, but some people will and that someone might be you. So I state this here so that you may understand the lengths that you may need to go to achieve the optimal balance.
As time has gone on my carbohydrate tolerance has improved as a byproduct of:
- Being more physically active
- Building more muscle mass (greater storage sites for glucose)
- Addressing nutrient deficiencies
- Addressing digestive health
- Improving toxic load
Which brings me to the next part of this blog which is other things that can be influencing blood sugar.
Your blood sugar may also be influenced by:
- Stress
- Caffeine
- A poor night’s sleep
- Food sensitivities (for me, cooked tomatoes always seem to spike my blood sugar, I’m not sure if that is histamine thing or just a thing)
- Nutrient deficiencies (like vitamin B6 and Chromium)
- Digestive imbalances
- Infections
- Toxic Load
- Inactivity
- Low muscle mass
Things you can do outside of dietary change to support blood sugar:
- Minimum 12 hour overnight fast
- Increase fasted window (nuance: fasting is not appropriate for everyone – learn more here)
- Move little and often (within your capacity) throughout the day. Even 1-2 minutes every hour can make a difference.
- Walk after meals for 15-30 minutes – provided this is in your capacity
- Cut out caffeine or only drink caffeine with meals
- Take a chromium supplement with a meal
- Support your nervous system and reduce stress
- Build muscle mass
- Address underlying imbalances and inflammation such as digestive issues, histamine intolerance or MCAS, food sensitivities, infections and toxic load
Supplements for Blood Sugar Control
These include:
- Chromium
- TUDCA
- Green Tea
- Alpha lipoic acid
- Myoinositol
- Berberine
Final words of wisdom
Working on fatigue recovery is a process. It can be overwhelming to work on too many things at once so take it one step at a time. Mastering blood sugar control is something that can make a big difference to your overall stability and resilience and this is exactly why it is one of the Foundational Five. If you want to learn more about the other Foundational Pillars and Blood Sugar Management specifically this is all covered in the Nurturing Resilience Membership. Take the Chronic Fatigue Quiz to learn which pillar is the most important for you right now.