Chronic pain, low mood and low energy are three things that often go hand in hand. Although these conditions are often not well supported with traditional medicine, they can be unravelled and addressed if you have the patience and commitment to do so.
The common thread that links all three is energy. Or, more specifically, ATP production. Impaired mitochondria increase oxidative stress leading to neuroinflammation and the inability to synthesise neurotransmitters. An inflamed and unhealthy brain can be more sensitive to the perception of pain and struggle to dampen pain signals.
As I have written previously on neuroinflammation and neurotransmitters and many of my previous blogs are centred around optimising energy production and mitochondrial function, here I will focus primarily on the understanding of the mechanisms which impact pain specifically – and how you can address them.
If you are someone who experiences chronic pain whether that is chronic migraine, headaches, neuropathic pain, fibromyalgia or pain linked with autoimmunity (e.g. Lupus or Rheumatoid), this is for you.
What is Pain: Understanding The Neurophysiology and Pathophysiology
Pain is an unpleasant sensory and emotional experience which makes it subjective and difficult to quantify and assess.
A nociceptor is a type of sensory receptor in the body that is responsible for detecting painful or potentially harmful stimuli such as heat, cold, pressure, or chemical irritants. When a nociceptor is activated by a stimulus, it sends signals to the brain that are interpreted as pain or discomfort.
Nociceptors are found throughout the body, including in the skin, muscles, joints, and internal organs, and they play an important role in the body’s ability to sense and respond to potentially harmful stimuli.
All pain is perceived in the brain; this means that if you are experiencing pain, then regions of the brain are firing. The experience of pain is created by:
- 1st order neurons connecting nociceptor to spinal cord (peripheral)
- 2nd order neurons connecting the spinal cord to brain (central)
- 3rd order neurons connect different regions of the brain (central)
Pain becomes chronic due to activation of the pain pathways or lack of activation of the inhibitory pathways or both.
Peripheral and Central Pain Sensitisation
Sensitisation is the underlying mechanism in chronic pain and pain syndromes. Peripheral and central sensitisation are two mechanisms by which chronic pain develops. Constant peripheral sensitisation becomes central sensitisation and then the two become a vicious cycle that needs to be untangled. They may be factors involved in chronic pain conditions, such as osteoarthritis, neuropathic pain, headaches and fibromyalgia.
Peripheral sensitisation refers to an increased sensitivity of nociceptors (pain receptors) in the peripheral nervous system, often due to tissue damage or inflammation. This can lead to an exaggerated or prolonged pain response to stimuli that would normally be perceived as only mildly painful or non-painful.
During peripheral sensitisation, the threshold for activation of nociceptors is lowered, so that they become more easily triggered by a stimulus. This can result in the transmission of more pain signals to the central nervous system (brain and spinal cord), leading to increased pain perception and sensitivity.
Central sensitisation is a phenomenon in which the central nervous system (CNS) becomes more sensitive to pain signals, leading to increased pain perception and sensitivity. This occurs when there is an amplification of pain signals in the CNS, particularly in the spinal cord and brain, due to changes in the function and structure of neurons involved in pain processing.
In central sensitisation, pain signals are transmitted to the CNS through nociceptors (pain receptors) in response to tissue damage or inflammation. These signals are then processed and amplified in the CNS, leading to an exaggerated and prolonged pain response.
This can cause pain to persist even after the original tissue damage or inflammation has resolved.
Descending Inhibitory Pathways
Pain inhibitory pathways are neural circuits in the central nervous system (CNS) that modulate the transmission of pain signals and help regulate pain perception. These pathways can act to reduce or block the transmission of pain signals, which can provide pain relief.
One of the main pain inhibitory pathways is the descending pain modulation pathway, which originates in the brainstem and sends signals down to the spinal cord. The brainstem releases neurotransmitters such as serotonin, norepinephrine and opioids, which act on receptors in the spinal cord to reduce the transmission of pain signals.
Other pain inhibitory pathways include the endogenous opioid system which involves the release of natural pain-relieving chemicals called endorphins and enkephalins, and the gamma-aminobutyric acid (GABA) system, which inhibits the activity of neurons involved in pain transmission.
Brain dysfunction is a common cause of poor pain inhibition pathways and therefore, a healthier brain will equate to a healthier pain management response.
Stress and Pain
When pain is activated in the body, the sympathetic nervous system is also activated. Therefore, it is inherently stressful to be in pain and yet stress also amplifies the experience of pain by releasing catecholamines (stress hormones) and causing constriction of blood vessels (i.e. poor blood flow and oxygenation of issues). Therefore, anyone who is experiencing chronic pain would also benefit from reducing sympathetic tone and increasing vagal tone. You can learn how to do this more specifically in the Nurturing Resilience Course.
Pain Sensitisation Amplifiers
Pain does not equal the amount of tissue damage. Instead, there may be physiological variables which can amplify pain signals and sensitise nociceptors. When working with chronic pain, it can be helpful to identify the specific amplifiers and have strategies to address them. These amplifiers include:
- Inflammation
- Prostaglandin and Leukotriene Imbalances
- Histamines
- Free Radicals and Oxidative Stress
- Adipokines (inflammatory molecules from excess body fat)
- Microbiome imbalances
- Neuroinflammation and substance P
- Hypoxia (poor oxygenation)
- Insulin Surges
- Stress Hormones / High Sympathetic Tone
- Advanced Glycation End Products (AGEs)
It is not uncommon for an individual to have more than one and therefore there are multiple triggers for nociceptors. For example, if you have an injury but you have higher amounts of histamine, blood sugar imbalances and high stress levels this can amplify the experience of pain.
How to Break The Cycle of Chronic Pain
To break the cycle you need:
- Energy in the form of ATP
- Decrease what is sensitising the peripheral nerves by addressing amplifiers
- Address the central sensitisation by restoring brain health. A healthier brain is more efficient at utilising the descending pathways that inhibit pain perception.
Inflammation
To relieve chronic pain we want to identify sources of inflammation in the body. This could be physical trauma / wear and tear, toxins, dietary proteins or infections (e.g. bacteria, parasites, mould, yeast or viruses)
In blood work we may see an increase in acute phase reactants such as CRP, Ferritin or ESR may increase when there is a lot of cytokine activity.
Prostaglandins & Leukotrienes
Prostaglandins and leukotrienes are types of eicosanoids, which are signalling molecules that are derived from arachidonic acid, a type of fatty acid found in cell membranes. They may have both a beneficial and inflammatory role.
Prostaglandins are involved in a wide range of physiological processes, including inflammation, pain, and fever. They are produced by various cells in the body, including immune cells, and act locally to promote inflammation and sensitise pain receptors (nociceptors). Prostaglandins also play a role in regulating blood flow, blood clotting, and the function of the gastrointestinal tract.
Leukotrienes, on the other hand, are mainly produced by immune cells and are involved in promoting inflammation and immune responses.
Both prostaglandins and leukotrienes are important mediators of inflammation and pain. Imbalances in these molecules may be driven by the balance of fatty acids in the diet. Someone who has an imbalance of prostaglandins and leukotrienes may want to reduce processed foods, red meat and dairy and increase olive oil, oily fish, nuts and seeds.
If aspirin helps your pain response this can be a clue that there may be a prostaglandin imbalance. A red cell fatty acid test from Genova Diagnostics can give further information about the balance of fatty acids in the diet.
Histamine
Histamine can cause hyperalgesia, which means that it changes pain perception, likely due to activating the microglial cells in the brain. High levels of histamine can be associated with pain, seasonal allergies, food allergies,cognitive dysfunction, brain fog, sensitivity to light and sound or intolerance to chemicals and smells.
It is a complex topic and you can learn about it in more detail here (MCAS, Histamine Intolerance and Chronic Fatigue)
Histamine may be an issues if eosinophils are elevated, blood histamine is high or there is elevated IgE (food, mold of chemicals). Parasitic infections can activate an IgE response, therefore, digestive health should also be considered. Getting pain under control will mean getting histamines under control.
Free Radicals and Oxidative Stress
The clue that free radicals and oxidative stress may be amplifying pain is if there is an increase in pain and inflammation with exercise. The body may hurt after exercise and cannot recover. In ME/CFS the body may lose function after exercise and there may be post-exertional malaise.
The solution in this case is to increase antioxidants and reduce exposure to things that may increase oxidative stress such as overtraining, cleaning chemicals, pesticides, toxins (e.g. mould mycotoxins), processed foods, air pollution, car exhaust fumes, radiation etc.
Elevated 8OHdG and lipid peroxides indicate need for antioxidants. This can be assessed with an Organic Acids Urine test such as the Metabolomix Test by Genova Diagnostics.
Hypoxia
Hypoxia is when not enough oxygen can get to the tissues. There may be many reasons for this including:
- Anaemia
- Sleep apnea
- Low blood pressure or high blood pressure
- Sedentary lifestyle
A simple test you can do is to buy a pulse oximeter. A pulse ox less than 94 can suggest that there is a problem getting oxygen to the tissues. You can the work backwards to establish a root cause.
Insulin Surges
Insulin is the hormone that increases after eating to transport glucose from the bloodstream into the cells. Metabolic dysfunction may be associated with postprandial insulin surges which can subjectively be identified if you experience fatigue after meals. Additionally, if your fasting insulin is elevated, if you have triglycerides (TGs) >1.7 mmol/L or a TG/HDL > 3, then insulin could be concern for you.
I am a big advocate of testing postprandial blood glucose as an early sign of metabolic dysfunction and insulin imbalances. You can learn how to do this here.
Advanced Glycation End Products (AGEs)
AGEs are a group of complex molecules that form when proteins or lipids (fats) are exposed to sugars (glucose) over a long period of time. This process, called glycation, occurs naturally in the body as we age, but it can be accelerated by a diet high in sugar, oxidative stress, and inflammation.
In the body, AGEs can accumulate in various tissues, such as the skin, blood vessels, and kidneys, leading to the development of chronic diseases. They can also stimulate the production of pro-inflammatory molecules, such as cytokines and chemokines, and promote oxidative stress, leading to tissue damage AND they can amplify pain signals.
Reducing AGEs in the body can be achieved by avoiding foods high in sugar, such as processed foods and sugary drinks, and by eating a healthy, balanced diet rich in fruits, vegetables, whole grains, and lean protein.
Certain cooking methods, such as grilling and frying, can also increase the formation of AGEs, so it is recommended to use cooking methods that are gentler, such as steaming or boiling.
Adipokines and Excess Body Fat
Our fat cells have the potential to release inflammatory cytokines known as adipokines. Adipokines are involved in regulating various physiological processes, including metabolism, inflammation, and immune function. Excess body fat has been associated with excess adipokine production and this may play a factor in the pain amplification.
Catecholamines
Catecholamines include adrenaline (epinephrine) and noradrenaline (norepinephrine), both of which can have a modulating effect on the nervous system either to amplify pain or relieve it.
Catecholamines are released by the sympathetic nervous system in response to stress. Generally, acute stress-induced release of catecholamines may produce analgesic effects, while chronic stress-induced release may produce hyperalgesic effects, contributing to the development and maintenance of chronic pain conditions.
The experience of chronic pain may further increase sympathetic tone and create a cycle of ongoing pain. Reducing sympathetic tone and increasing vagal tone may support pain management but in order for this to happen we need a healthy brain.
An unhealthy brain cannot suppress sympathetic activation and this can cause light and sound sensitivity, chronic pain and other symptoms.
Substance P and Neuroinflammation
Substance P is a neuropeptide that functions as a neurotransmitter and neuromodulator in the nervous system. It is widely distributed throughout the central and peripheral nervous systems.
Substance P acts as a pro-inflammatory neuropeptide that sensitises pain-sensing neurons and enhances the transmission of pain signals to the brain. Substance P is released in response to tissue damage, inflammation and other noxious stimuli
In addition to its role in pain perception, substance P is also involved in other physiological processes, such as inflammation, neurogenesis, and mood regulation. It has been implicated in the pathophysiology of various conditions, such as migraine headaches, chronic pain, depression, and anxiety disorders.
Neuroinflammation can increase the expression and release of substance P and therefore, part of modulating pain is managing neuroinflammation to reduce substance P expression.
Low Cortisol
Cortisol is an anti-inflammatory hormone, therefore if cortisol production is blunted, the body may not be able to dampen and complete inflammatory responses associated with chronic pain.
The body’s cortisol response can be assessed with saliva cortisol testing.
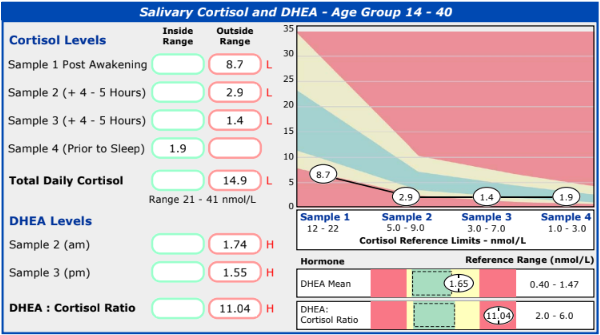
People with low cortisol may also experience difficulty regulating their blood sugar and be prone to hypoglycemia (low blood sugar). Low blood sugar puts further strain on the adrenal glands which perpetuates the cycle. Therefore, stabilising blood sugar, the nervous system and supporting the adrenal glands may be important for managing chronic pain.
Intestinal Permeability
Intestinal permeability is colloquially known as “leaky gut”. It refers to the abnormal increase in the permeability of the intestinal lining, which can allow the passage of toxins, bacteria, and other harmful substances into the bloodstream.
This can trigger an immune response and inflammation in the body, which can contribute to the development of chronic pain. When there is an overgrowth of gram negative bacteria in the gastrointestinal tract, these bacteria produce endotoxins known as lipopolysaccharides (LPS).
LPS can pass through a permeable membrane into the bloodstream causing systemic inflammation which can contribute to the development and maintenance of chronic pain conditions.
There is increasing evidence to suggest that intestinal permeability and gut dysbiosis are associated with chronic pain conditions, such as fibromyalgia, irritable bowel syndrome (IBS), and chronic fatigue syndrome. In some cases, interventions aimed at restoring gut health, such as dietary changes, probiotics, and prebiotics, have been shown to improve symptoms of chronic pain, although more research is needed to fully understand the mechanisms underlying these effects.
Brain Function
A healthy brain has health pain modulation. What does the brain need to be healthy?
- Sleep
- Fuel; balanced blood sugar or ketones
- Oxygen and blood flow
- Movement and Exercise
- Healthy anti-inflammatory fats such as EPA and DHA found in oily fish and algae
Natural Opioids
To alleviate chronic pain we want to dampen nociceptors and increase natural opioids.
Medicinal opioids help dampen pain but lead to increased central sensitisation. Therefore, in the long term, you will need to take more and more to have the same effect.
Natural endogenous opioids do not have that effect, these include:
- Pets
- Sex
- Massage
- Exercise
- Laughter
- Yoga
- Meditation
- Visualisation
Conclusion
Unravelling the vicious cycle of chronic pain, low energy and low mood is not quick and easy but it is possible. The most important factors are:
- Increasing energy
- Dampening pain signals by identifying and addressing amplifiers
- Improving brain health for central sensitisation and
- Increasing opioids to dampen pain signals
It will take time and a methodical plan. If you would like help with that plan, consider working with me either in the Fatigue Recovery Road Map and 1-1 Six Month Support Plan. You can find out more about these two options here.