The Importance of Oxygen for Energy
Humans need oxygen to survive. That is an absolute fact. Therefore, it should come as no surprise that anaemia and poor oxygen delivery are very important to address in chronic illness generally and fatigue recovery specifically. However, this is an often overlooked, under-assessed and under addressed aspect of health.
We burn fat in the presence of oxygen to make our energy currency, ATP. For every molecule of glucose that we consume we can make 2 ATP without oxygen but we can make up to 38 ATP when we use oxygen in the citric acid cycle and transport electrons along the electron transport chain on the mitochondrial membrane.
Therefore, being able to transport oxygen to our cells is a very important part of energy production. And fatigue ultimately comes down to an inability to make enough ATP to meet our needs.
Red blood cells are the body’s oxygen transporters and therefore, an understanding and assessment of red blood cell number and size is an essential component of any fatigue case.
Signs of Anaemia / Poor Oxygenation
Red blood cells are the body’s oxygen transporters and therefore, an understanding and assessment of red blood cell number and size is an essential component of any fatigue case.
When we are not effectively getting oxygen where it needs to go in the body we may experience:
- Fatigue
- Weakness
- Headaches
- Poor exercise tolerance
- Problems thinking and concentrating
- Irritability
- Loss of appetite
- Numbness and tingling in the hands and feet
- Poor circulation to the extremities e.g. cold hands and feet
- Brittle nails
- Blue colour to the whites of the eyes
- Desire to eat ice or other non-food things (known as pica syndrome)
- Feeling lightheaded when moving from sitting to standing
- Pale skin tone
- Shortness of breath with mild activity or even rest
- A sore or inflamed tongue or mouth
- Abnormal or increased menstrual bleeding in women
- Mouth Ulcers
If you are experiencing any of these symptoms you should see your doctor who will be able to support you with relevant testing.
Red Blood Cells
The Red Cells are important oxygen transporters and changes in red blood cells number and size will impact oxygen delivery and energy. The good news is that we can assess red blood using basic blood testing in the form of a Full Blood Count.
A Full Blood Count may look as follows:
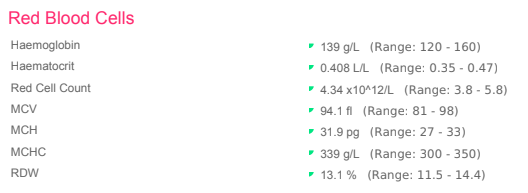
Low levels of the top three markers reveal if there is anaemia:
- ↓ Haemoglobin (Hb)
- ↓ Haematocrit (HCT)
- ↓ Red Blood Cells (RBC)
The lower three markers can reveal what type of anaemia is present. For example:
- MCV
- Normal = normocytic
- Depressed = microcytic
- Elevated = megaloblastic
- MCH and MCHC
- Normal = normochromic
- Depressed = hypochromic
- Elevated = megaloblastic
Table 1: Shows the different types of anaemia and how this may present in a full blood count
| Microcytic Hypochromic Anaemia | Normocytic Normochromic | Megaloblastic Anaemia | |
| Hb, HCT, RBC | ↓ | ↓ | ↓ |
| MCH, MCHC | ↓ | Normal | ↑ |
| MCV | ↓ | Normal | ↑ |
| Associated with | Iron deficiency, anaemia from blood loss, anaemia of chronic disease and inflammation, sideroblastic anaemia, thalassemia | Chronic inflammation and disease and anaemia of acute and chronic blood loss, hemolytic anaemia, anaemia secondary to renal disease, and others… | Need for vitamin B12, folate or pernicious anaemia which is an autoimmune condition affecting intrinsic factor. |
Iron Deficiency
There are 3 stages of iron deficiency:
- Stage 1 Iron Depletion, reflected in low ferritin only
- Stage 2 Iron Deficiency, reflected in low ferritin, low iron, low iron saturation, increased TIBC, increased Transferrin but a normal Full Blood Count
- Stage 3 Iron Deficiency Anaemia whereby the Full Blood Count is now impacted to reflect ↓ Hb, HCT, RBC, MCH, MCHC, MCV and an increased RDW
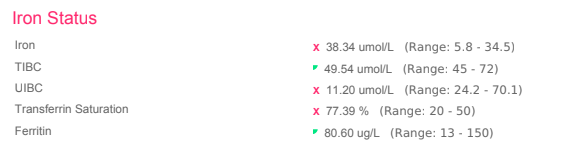
Therefore, to identify patterns of iron deficiency before someone becomes fully anaemic we want to run a full iron panel which includes:
- Ferritin
- Total Iron
- Iron Saturation %
- Transferrin
- TIBC
If a pattern of iron depletion, iron deficiency or stage 3 iron deficiency anaemia is identified we want to ask the question: why?
Common Causes of Iron Deficiency and Depletion
Poor Dietary Intake
This is common in vegan or vegetarian diets, under-eating or disordered eating.
Situations Where Tissue Growth Exceeds Iron Intake
This is possible in pregnancy, uterine fibroids and colon cancer.
Loss of Iron is Greater Than Intake
This is common in women who are affected by heavy periods. Iron supplementation may be required in the short term to replace iron lost in menstruation but long term we want to stabilise and optimise menstrual flow. You can read more about this in my previous post where I discuss oestrogen dominance, a common cause of heavy periods.
Other causes may be internal bleeding, an ulcer, colon cancer.
Poor Iron Absorption
This is possible when stomach acid is low, celiac disease, increased intestinal permeability (leaky gut), intestinal parasites or infections such as H.pylori.
Parasites
I frequently find parasites when using stool tests with my clients. Even when parasites have not been identified in stool testing many of my clients and self included, will pass worms in their stools when taking a Full Moon Parasite Cleanse. (although you can purchase the cleanse through Amrita using my code 2IF3B6, this is not something you want to throw yourself into without proper preparation.
Low Stomach Acid
If low stomach acid is suspected one may experience symptoms such as bloating, gas and flatulence shortly after eating. There may be undigested food in the stools and other gastrointestinal symptoms such as stomach pains, constipation, diarrhoea or diarrhoea shortly after meals. Other symptoms may include bad breath, loss of the taste for meat, a sense of fullness after meals, fingernails which chip and peel or break easily. There may be unresponsiveness to iron supplementation.
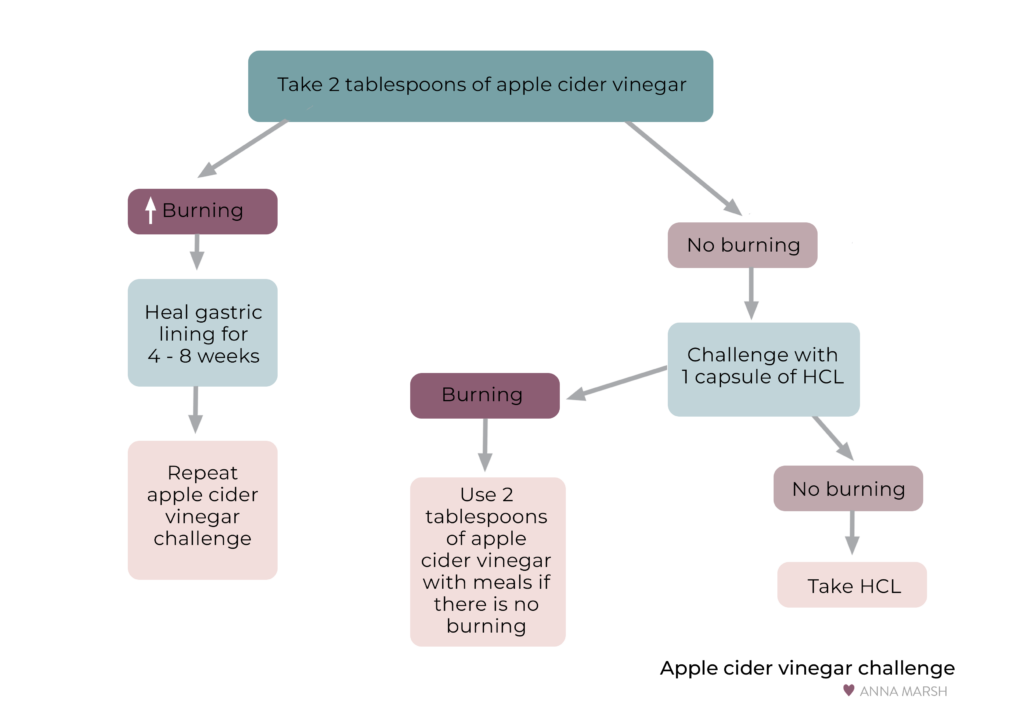
If you suspect that you may have low stomach acid you can complete the Apple Cider Vinegar Challenge under the guidance of your practitioner. The challenge, depicted in the image below, is designed to challenge the stomach’s capacity for acid. This is first done by consuming 2 Tbsp of apple cider vinegar on an empty stomach. I recommend that this is done 5-10 minutes before a meal so that you can eat your meal to offset any heartburn should this be your experience.
If a burning sensation is experienced after challenging with the vinegar, the stomach may in fact have a high level of acidity and further support may be needed in this regard. No burning may suggest low acidity and the next step would be to challenge with Betaine HCl and Pepsin. The number of capsules of Betaine HCl and Pepsin taken with a meal can be titrated upwards until a burning sensation is achieved and then this dosage minus 1 capsule can be taken to support optimal digestion of important nutrients, like iron.
Dietary Iron
If dietary intake of iron is the issue, this would be the first thing to address. Here are the best dietary sources of iron, presented in order based on iron content.
Iron Rich Food Sources
Liver, beef, turkey, venison, sardines, seafood, eggs,
Vegetarian sources: soybeans, lentils, tofu, blackstrap molasses, quinoa, chickpeas, pinto beans, black eyed peas, swiss chard, tempeh, black beans, turnip greens, prune juice, spinach, beet greens, tahini, lima beans, sunflower seeds, dried figs, dried apricots.
Vitamin C supports iron absorption
Red chilli peppers, guava, sweet red peppers, kale leaves, parsley, collard greens, turnip greens, broccoli, brussels sprouts, mustard greens.
Heme iron is found in animal produce and non-heme iron is found in plants. Heme iron is well absorbed and nonheme iron is less well absorbed. Therefore, my preference for clients who need to build up their iron levels is to have them consume liver and high quality animal produce.
If this is not possible, then I would recommend an iron supplement.
Iron Supplementation
I normally recommend an Iron Bisglycinate supplement with liver extract in capsule form being an alternative option. This is dosed at 2x25mg every other day as there is some research to suggest that this supports absorption. This should be ideally taken with some vitamin C on an empty stomach, away from other foods and drinks for best absorption.
Recommended iron intake for non-pregnant menstruating women is 20mg/d but this does not account for other factors such as poor absorption or increased blood loss so I recommend regular monitoring of an iron panel and full blood count to assess the efficacy.
Factors that may inhibit iron absorption
- Coffee, tea, milk, cereals, dietary fibre, carbonated beverages which contain phosphate
- Multivitamins or supplements that contain calcium, zinc, manganese or copper
- Antacids, H2 Blockers or proton pump inhibitors
- Quinolones and tetracycline antibiotics
Other possible causes of Microcytic Hypochromic Anaemia
Anaemia may not always be related to nutrient deficiencies and therefore it is important to understand other causes or red blood cell and iron panel abnormalities.
Anaemia of Inflammatory Disease
Anaemia of chronic disease and inflammation happen inflammation drives up inflammatory cytokines which activate the liver’s production of hepcidin. Hepcidin then influences the bone marrow, intestines, kidneys and macrophages (immune molecules). The result effects are:
- A shift in RBC production to WBC production in the bone marrow
- Macrophages suppress iron release
- Kidneys suppress EPO which results in less stimulation to the bone marrow for RBC production
This might show up as:
- ↓ RBC, Hgb, HCT
- Normal MCV, MCH, MCHC, RDW
- Iron = Normal
- Ferritin = Normal range to elevated
- TIBC = Normal range to elevated
- Transferrin = Normal range to depressed
As this progresses:
- ↓ RBC, Hgb, HCT
- ↓ MCV, MCH, MCHC
- RDW = Normal or elevated
- Iron = Normal
- Ferritin = Normal range to elevated
- TIBC = Normal range to elevated
- Transferrin = Normal range to depressed
When there is a combination of Iron Deficiency Anaemia and Anaemia of Inflammation / Chronic Disease:
- Iron Saturation = Normal to Depressed
- Ferritin = Normal, elevated or depressed
- TIBC = Normal, depressed or elevated
- Transferrin = Normal, depressed or elevated
- Soluble transferrin receptor (sTfr) = elevated
- sTfr / Ferritin ratio = <1 for anaemia of chronic disease
- sTfr / Ferritin ratio = <2 for a mixed pattern
Anaemia of Blood Loss
Blood loss can be acute or chronic and there may be clues that show up in one’s blood that reveal which is which.
Anaemia of Acute Blood Loss
- ↓ RBC, Hgb, HCT
- Normal MCV, MCH, MCHC, RDW
- Normal Ferritin, Iron, Iron Saturation and TIBC
- Elevated Reticulocytes
- Reticulocyte production index >2%
Anaemia of Non-Acute Blood Loss
- ↓ RBC, Hgb, HCT
- ↓ MCV, MCH, MCHC
- RDW = normal or elevated
- Ferritin = normal
- Iron = normal to depressed
- Iron Saturation = normal to depressed
- TIBC = = normal to elevated
- Elevated Reticulocytes
- Reticulocyte production index >2%
Sideroblastic Anaemia
Sideroblastic anaemia is condition where the body produces enough iron but is unable to make adequate haemoglobin due to an increased need for vitamin B6, toxins such as lead, copper and zinc and genetic deficiencies.
The consequence is that iron accumulates in the mitochondria or in the body which can lead to an enlarged spleen, liver or systemic inflammation.
Sideroblastic Anaemia can be identified by:
- ↓ RBC, Hgb, HCT
- ↓ MCV, MCH, MCHC
- ↑ RDW
- ↑ Iron
- ↑ Iron Saturation
- ↑ Ferritin
- TIBC = normal
- Transferrin = normal
Addressing Sideroblastic Anaemia can include:
- High amounts of vitamin B6
- Removal of vitamin B6 depletion (alcohol and medication)
- Bone marrow transplant in severe cases
- Low iron diet or deferoxamine for iron overload
Thalasemia
This is a genetic disorder where the body doesn’t make adequate haemoglobin. It can be managed with transfusions and chelation therapy.
Megaloblastic Anaemia (Vitamin B12 and Folate Deficiency)
Megaloblastic anaemia is characterised by:
- ↓ Hb, HCT, RBC
- ↑ MCH, MCHC
- ↑ MCV
- Associated with the need for vitamin B12, folate or pernicious anaemia which is an autoimmune condition affecting intrinsic factor.
If megaloblastic anaemia is identified then intrinsic factor antibody testing can be used to rule out autoimmunity. If antibody testing is negative then one must consider if the issue lies with a dietary need for folate and/or B12 or if there may be another reason for compromised absorption or loss of these nutrients.
An organic acids test can give further information about whether or not the need is for vitamin B12 specifically or folate specifically or a combination of the two. The markers associated with B12 and folate are methylmalonic acid and FIGLU respectively.
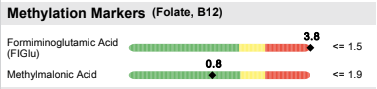
In this case FIGLU is elevated but methylmalonic acid is in the green zone suggesting that the issue lies with folate specifically.
Homocysteine and Cystathionine can be other useful markers of B12 and Folate status.
If low B12 and / or folate is identified the approach would be:
- Rule out Antibodies to Intrinsic Factor
- Rule out Hypochlorhydria (e.g. Apple Cider Vinegar Challenge) and digestive imbalances impacting absorption (e.g. infections or use of PPIs)
- Address intake with supplementation and dietary intake
For the most part, unless someone is a vegan or vegetarian and not supplementing with vitamin B12, the most common cause will be the inability to absorb.
B12 Rich Food Sources
B12 comes from animal produce, especially liver, sardines, snapper, venison, shrimp, scallops, beef, lamb, cod, halibut, eggs, cheese (especially cottage cheese), milk, yoghurt, turkey, brewers yeast. It can also be made in the gut. We’ll touch on gut health later, but I often recommend 1-2 servings of fermented foods per day.
- Coconut Kefir
- Kimchi
- Sauerkraut
- Kombucha
There are no vegetarian or vegan sources of B12 so taking a supplement can be helpful in this case.
Folate Rich Food Sources
Romaine lettuce, spinach, asparagus, liver, parsley, kelp, spring greens, broccoli, cauliflower, celery, lentils, Brussel sprouts, pinto beans, black beans, chickpeas, kidney beans, navy beans, green beans and cabbage.
Folate can also be supplemented, the individual dosage requirements can vary therefore I recommend working with a practitioner who can guide you in your dosage and help you navigate ongoing monitoring.
Appendix – Reference Ranges
Table 2: The following are the optimal and alarm reference ranges as suggested by Weatherby and Ferguson in their book, Blood Chemistry and CBC Analysis.
| Marker | Optimal Range | Alarm Range |
| Red Blood Cells (RBC) | Men: 4.2- 4.9 x1012/L Women: 4.0 – 4.5 x1012/L | < 3.8 x1012/L< 3.5 x1012/L |
| Haemoglobin (Hb) | Men: 140 – 150g/L Women: 135 – 145g/L | <100g/L |
| Haematocrit (HCT) | Men: 0.4 – 0.48 Women: 0.37 – 0.44 | < 0.32< 0.32 |
| MCV | 82.0 – 89.9 fL | < 78.0 or > 95.5 fL |
| MCHC | 0.32 – 0.36 | n/a |
| MCH | 28.0 – 31.9 pg | < 24.0 or >34.0pg |
| RDW | <13% | n/a |
| Ferritin | Men: 33-236 ug/L Women Before Menopause:10-122 ug/L* After Menopause:10 – 236 ug/L* | <8ug/L or > 500ug/L |
| Serum Iron | 8.96 – 17.91 umol/L | <4.5 or > 35.82 umol/L |
| TIBC | 44.8 – 62.7 umol/L | n/a |
| Transferrin Saturation % | 20-35% | <5% or >70% |
*The reference range for ferritin is very large. Optimal for fatigue is suggested to be around 50 ug/L
Final Words
There can be a lot of complexity and detail required when it comes to making a proper assessment in chronic illness and fatigue cases. If you would like help understanding your needs and what to prioritise in your healing journey, you can find out more about working together here.