Chronic Fatigue can be the end point of a complex web of dysfunction leading to poor ATP production. Malabsorption Syndromes can be part of the web that needs to be untangled as someone works to improve their health, energy and wellbeing.
Malabsorption syndrome refers to a group of disorders that affect the body’s ability to properly absorb nutrients, vitamins, minerals, and other important substances from the food you eat. This condition occurs when the digestive system, particularly the small intestine, is unable to absorb nutrients effectively.
Mechanisms of Malabsorption Syndromes and Chronic Fatigue
There are several mechanisms that link malabsorption syndromes to chronic fatigue. These include:
Nutrient Deficiencies
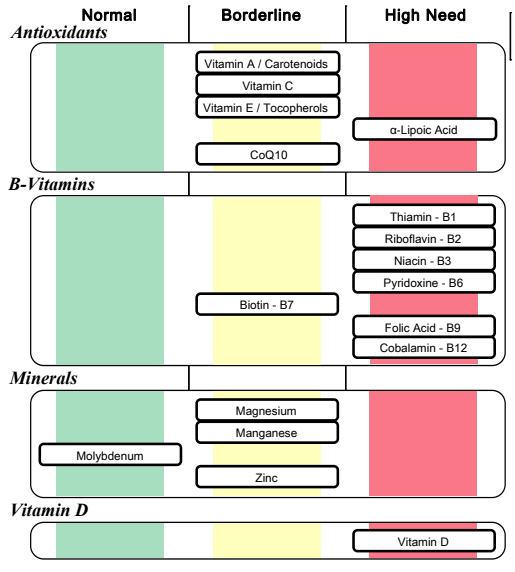
Malabsorption syndromes can lead to deficiencies in essential nutrients such as vitamins (e.g., B vitamins, vitamin D, vitamin K) and minerals (e.g., iron, magnesium). These nutrients play critical roles in energy production, immune function, and overall bodily processes. A lack of these nutrients can lead to fatigue and a general feeling of weakness.
Anaemia
Malabsorption of iron and vitamin B12 can lead to anaemia. Anaemia is characterised by a reduced number of red blood cells or a decrease in haemoglobin levels. Haemoglobin carries oxygen to cells throughout the body, and when it’s low, tissues and organs, including muscles and the brain, may not receive sufficient oxygen, leading to fatigue.
Impaired Energy Metabolism
Malabsorption can disrupt the body’s ability to break down and absorb carbohydrates, fats, and proteins. These macronutrients are crucial for producing energy through metabolic processes. If they are not properly absorbed, the body may struggle to generate enough energy, resulting in fatigue.
Reduced Nutrient Transport
Malabsorption can affect the transport of nutrients across the intestinal lining into the bloodstream. This can lead to an inadequate supply of nutrients to various tissues and organs, including the muscles and brain, causing fatigue and reduced cognitive function.
Disrupted Hormonal Balance
Malabsorption can also impact the hormonal balance within the body, including hormones that regulate metabolism, energy levels, and overall well-being. Hormonal imbalances can contribute to feelings of fatigue and low energy.
Gut Inflammation and Immune Response
Many malabsorption syndromes are associated with inflammation and immune responses in the gut. Chronic inflammation can trigger a systemic response, leading to fatigue and a sense of tiredness.
How To Assess If a Malabsorption Syndrome Is a Factor In Your Chronic Fatigue?
Symptoms of malabsorption syndrome can vary widely but often include:
- Diarrhoea
- Weight loss or inability to gain weight due to muscle wasting
- Abdominal pain or discomfort
- Bloating and gas
- Weakness and fatigue
- Vitamin and mineral deficiencies, leading to various complications like anaemia, osteoporosis, and neurological problems
- Deep muscle or bone pain
- Chronic muscle spasms
- Easy bruising and bleeding gums
- Loss of menstrual cycles in women
- Abnormal stools; blood in stools, steatorrhea, clay coloured stools
- Inflammation of the tongue or coated tongue
- History of Autoimmune disease
A simple blood test is a good place to start, specifically looking for markers which may be out of balance. These include:
- Signs of anaemia (typically low red blood cells, haemoglobin, haematocrit and increased MCV, MCH, MCHC)
- Low Cholesterol
- Decreased albumin, globulin or protein
- Low platelet count and vitamin D, despite supplementation – which can suggest poor absorption of fat soluble nutrients, ADEK
These would be your initial clues that a malabsorption syndrome may be a concern. However, once you suspect a malabsorption syndrome, you must identify the underlying cause and address it.
Depending on the severity of the case, malabsorption syndromes may be chronic and require life long support to stabilise symptoms and maintain quality of life.
Possible Causes of Malabsorption Syndrome
The 4 main cause of malabsorption syndromes are:
- Damage to the Brush Border Microvilli of the Small Intestine
- Gallbladder and bile dysfunction:
- Poor gallbladder contraction
- Poor bile salt production
- Poor bile salt reabsorption
- Chronic Pancreatic Disease; inability to produce digestive enzymes causing fat, protein and carbohydrate malabsorption
- Reduce circulation to the intestine due to congestive heart failure
If you are impacted by 3 & 4 your case should be overseen by a medical doctor. Therefore, it is beyond the scope of this blog to discuss further details. But we will dive deeper into 1 & 2.
Damage to the Brush Border Microvilli
Common causes of brush border damage are:
- Celiac Disease
- Chronic Inflammatory Bowel Disease
- Small Intestinal Bacterial Overgrowth
- Radiation Treatment
- Intestinal Autoimmunity
- Intestinal Infections
Celiac Disease
An autoimmune disorder where the ingestion of gluten triggers an immune response that damages the lining of the small intestine, leading to impaired nutrient absorption. The best test for Celiac Disease is Cyrex Array 3, which tests for several different immune reactions to gluten and wheat, including transglutaminase 2 antibodies. Transglutaminase 2 antibodies cross react with gluten to destroy the microvilli of the small intestine. This impacts the integrity of the intestinal membrane and the ability to produce brush border enzymes responsible for food digestion. Advanced stage celiac disease can be determined but endoscopy where atrophy of the microvilli may be visible.
It can be helpful to test for Transglutaminase because gluten cross-reacts with other foods, known as gluten cross-reactive foods. When there is a cross-reaction between gluten and another food, continuing to eat the gluten cross-reactive food may continue to destroy the microvilli, even when eating gluten free.
Intestinal Autoimmune Diseases
Intestinal Autoimmune Diseases include Crohn’s Disease, Ulcerative Colitis and Autoimmune Gastritis. Testing for these includes the following:
- Crohn’s disease: Anti-Saccharomyces cerevisiae antibodies (ACSA) and endoscopy
- Ulcerative Colitis: Antineutrophil Cytoplasmic Antibodies (ANCA) and sigmoidoscope (Ulcerative Colitis)
- Autoimmune Gastritis: Anti-parietal Cell Antibodies and endoscopy
When autoimmunity is suspected it can be helpful to run Cyrex Array 5 which tests for 24 different auto antibodies that could be impacting several body tissues. If autoimmunity is positive, the digestive system may need specific support and the body as a whole may need support specific to autoimmunity which goes beyond the scope of this blog.
Parasitic Infections
Certain parasites can damage the intestinal lining and interfere with nutrient absorption. Parasites can be identified in stool testing and elevated eosinophils (>3%) in a Full Blood Count. You can read more here about how to assess and address parasite infections.
Small Intestinal Bacterial Overgrowth (SIBO)
SIBO is a condition where there is an abnormal increase in the number and/or types of bacteria in the small intestine. These bacteria can interfere with the normal digestion and absorption of nutrients, leading to malabsorption.
SIBO can be identified with breath testing. If there is a positive result, traditional support normally looks like antibiotic or natural antimicrobial therapy in conjunction with a low FODMAP diet. This can be successful in some cases but some people may be prone to recurrence when underlying factors are not acknowledged and addressed. This might include:
- Addressing stomach acid
- Addressing the nervous system
- Addressing neuroinflammation
- Addressing the gut-plexus and enteric nervous system
It is critical that SIBO is appropriately addressed to prevent ongoing destruction of the microvilli and associated malabsorption.
Gall Bladder Dysfunction
The gallbladder is where bile salts are made and released into the gut. In the gut, bile salts emulsify fats allowing for the absorption of fatty acids and fat soluble nutrients like vitamins ADEK.
Suspect gallbladder dysfunction when:
- Cholesterol is low
- Vitamin D is low despite supplementation
- When platelets are low
- There may be intolerance to fatty meals or “fish burps” when eating oily fish or taking fish oil supplements.
- Upper back and abdominal pain
Impaired synthesis of bile salts can lead to bile sludge and gallstones. Poor gallbladder contractility means that bile salts are not ejected into the gut which not only impacts fat digestion and absorption of important nutrients, but the balance of the microbiome.
Gallbladder contractility can be increased with exercise and vagal stimulation and sometimes further underlying imbalances may need to be addressed such as:
- Medications that increase risk (Hormone Replacement Therapy, Oral Contraceptives, Statins, Diuretics and Chronic Use of Antibiotics)
- Chronic intestinal inflammation
- Gut neurodegeneration
- Brain Injury
- Neurodegenerative disease
- Iron deficiency (leads to cholesterol saturation of stones and reduces gallbladder motility)
The Following Nutraceuticals May Be Useful
| Nutraceutical | Mechanism of Action |
| Coffee Green Tea Ginger Curcumin | Promotes gallbladder contraction, motility and ejection |
| Phosphatidylcholine Beetroot extract Taurine Vitamin C | Promotes metabolism of cholesterol on bile salts |
| Milk Thistle Dandelion | Counteracts the negative impact of oestrogen on bile flow |
| Bile Salts (ox bile) | Dissolves gallstones aggressively |
My Personal Story With Malabsorption
In my own journey to recovery from Chronic Fatigue Syndrome and Mould Illness, malabsorption was one of the challenges that I faced. I’d like to share some of my own story here to bring this information to life.
In my journey I experienced chronic diarrhoea which presented as watery stools up to 15 times per day for almost 2 years. This was better in certain parts of my menstrual cycle and worse when hormones were lower (e.g follicular phase of the cycle).
I did many tests and took many many different combinations of supplements and failed many times. I’d like to share some test results and what helped me the most in my case.
The first test that relevant to my digestion was the GI Effects offered by Genova Diagnostic (retails around £375).
Summary of Results:
- Several Infections – yeast, parasites
- Dysbiosis (bacterial overgrowth)
- Maldigestion
- Inflammation
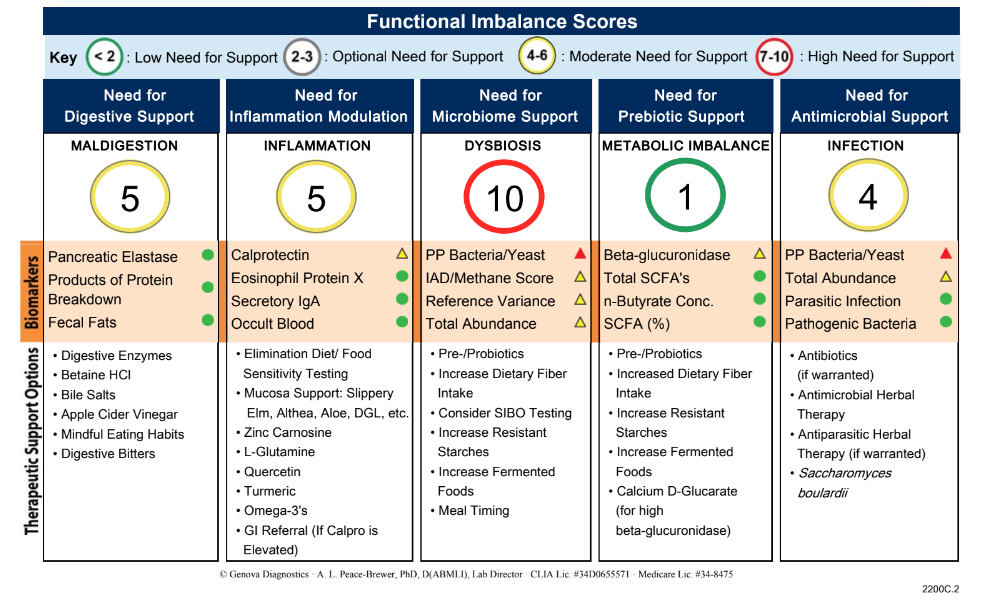
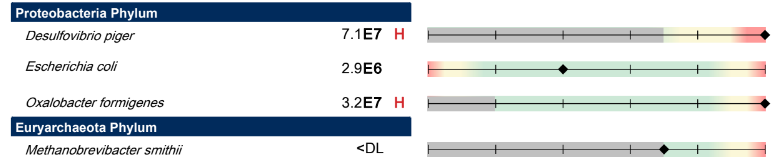
I had a large amount of Desulfovibrio piger which is a specific bacteria associated with Hydrogen Sulfide SIBO, which has been linked more so with diarrhoea. I had low levels of Methanobrevibacter smithii. Hydrogen sulfide SIBO is difficult to test so I didn’t do a SIBO breath test in this case. I often do not do SIBO breath testing with clients either, we test to assume that it is there and put more attention on working out why it is there so that it doesn’t become recurrent.
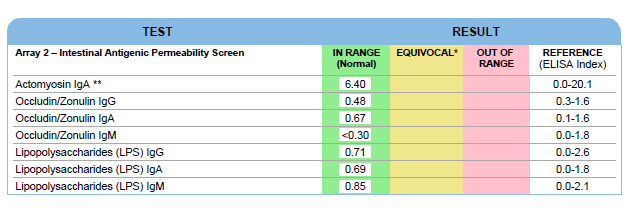
Due to the extent of my dysbiosis I also did Cyrex Array 2 to test for intestinal permeability (leaky gut) and endotoxemia, which is when bacterial toxins translocate into the bloodstream, attach to immune receptors called Toll-like receptors (TLRs) and create systemic inflammation. Fortunately the results all came back negative which was a blessing as I am sure I would have felt much worse if I had intestinal permeability and endotoxemia.
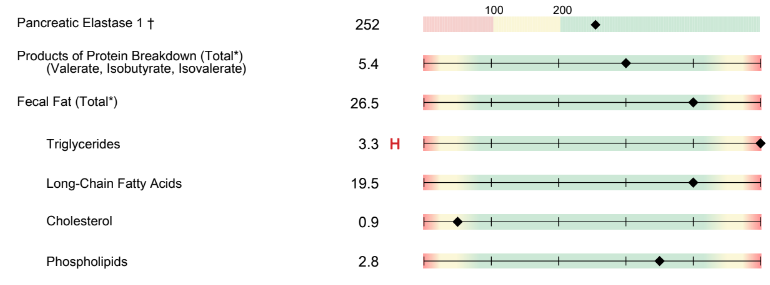
I also had elevated faecal fats and although pancreatic elastase was in the green, I would still consider this low for someone of my age.
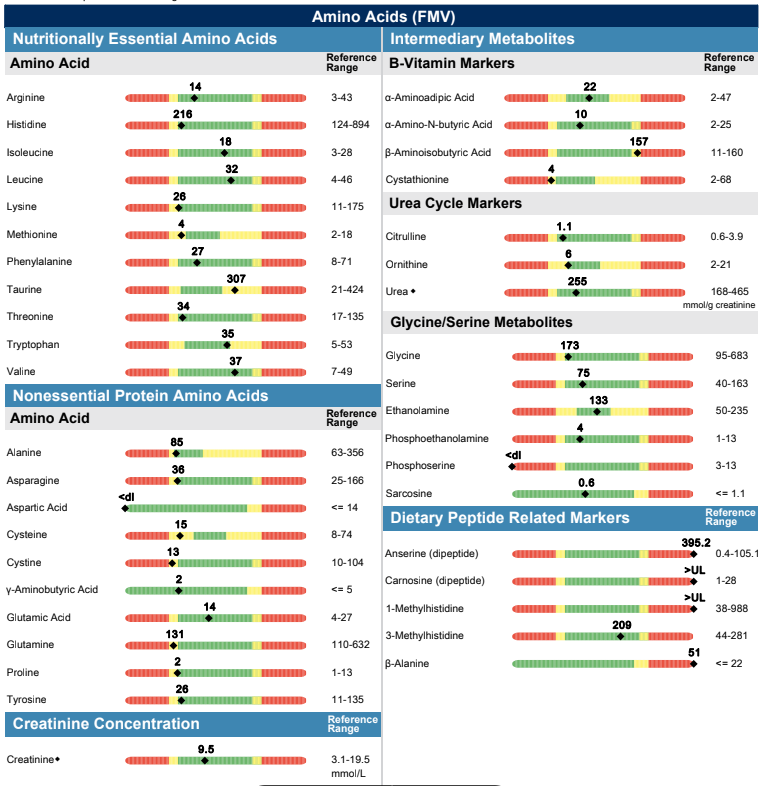
I did this stool test in October 2020. In January 2021 I did a NutrEval which showed the extent of my nutrient depletion – I needed everything.
Protein markers were all looking a little low…
And my bloodwork showed both low albumin and globulin

What did I do to address the Malabsorption?
After trying many different combinations of supplements the things that made the biggest difference for me were:
- Brain Retraining + Somatic Nervous System Work – I offer both these skills in my Nurturing Resilience Program
- A low sulfur diet
- Oregano and Bismuth to address SIBO
- Betaine Hydrochloride and Digestive Enzymes
- Probiotics
- Parasite Cleansing
This took place over more than 12 months with several cycles of support. If I was to place it on a timeline, it would look as follows:
January 2021 – Started Somatic Work
March 2021 – June 2021 – 3 months Brain Retraining
May 2021- July 2021 Bismuth, Oregano, Digestive Enzymes and Betaine Hydrochloride, Low Sulphur Diet where I excluded low sulphur vegetables but not proteins. My diet was ketogenic during this time. I followed this template from Dr Ruscio.
During this time my digestion stabilised for the first time in almost 2 years and I was able to grow my exercise tolerance and overall capacity as a result.
July 2021+ Probiotics
March 2022 – Liver Cleanse
March 2022, April 2022, May 2022 – Monthly Full Moon Parasite Cleanse
June 2022 – Oregano and Digestive Enzymes + Betaine Hydrochloride
Ongoing probiotics and parasite cleanses
Able to reintroduce high sulphur foods – I now eat raw onions and garlic!
This was my journey, but everyone will have a different journey depending on their unique case. My hope for sharing my journey is to give you insight into how you can work with a practitioner to interpret test results and make clinical decisions. Additionally, it takes time and maybe a few rounds of doing different things to get an end result.
Recently I went out for a meal while on holiday and I suspect I picked up some sort of infection as my diarrhoea symptoms returned, although not as severe as they were in the height of my illness. Fortunately with the addition of a few supplements I was able to rebalance my gut pretty quickly without experiencing any downturn in my overall health.