Stability is the first step in Chronic Fatigue Recovery. If you are someone experiencing a chronic illness such as CFS/ME, Long Covid, Post-Viral Fatigue, Vaccine Injury, Fibromyalgia or an autoimmune condition, you will be very familiar with the concept of energy crashes, symptom flares and post-exertional malaise (PEM) – all of which are symptoms of an unstable system.
This instability can be found in the physiology of the individual and has likely manifested over time due to the accumulation of chronic stress that has not been able to settle or discharge in the person’s nervous system. An unstable system has poor resilience to cope with stress and is highly sensitive to change or even positive and fun experiences.
You may reflect back on how you became unwell and for some, there may have been a gradual loss of resilience over time i.e. becoming less and less stress tolerant and needing more and more self care to continue to function as the years pass (this was my experience). For others, there may have been an acute event that happened (e.g. a viral infection) that was so significant that it threw your system completely out of balance.
Whether your experience was a slow burn or a sudden onset, the goal in the early stages of chronic fatigue recovery is to support the body to come back to a better sense of balance and stability.
The Pillars of Stability
When working with clients on their Chronic Fatigue Recovery, the goal is to identify and support those factors that will help the individual stabilise. Working with clients with complex and chronic illness you learn pretty quickly that every case is different and each person presents with their own set of unique challenges.
That being said, from experience I have been able to identify the most common factors that will help the individual stabilise the system most effectively. These are:
- Stabilising the Nervous System
- Stabilising Blood Sugar Balance
- Stabilising Sleep and Circadian Rhythms
- Stabilising energy output i.e. pacing and movement routines
- In some, but not all cases, we may need to stabilise the body if there is an active infection, particularly gut infections, although this is where the nuance comes in
I’ll go into further details on each of these below.
Stabilising The Nervous System
I could write a whole blog on the nervous system and I would still be scratching the surface of everything that I would want you to know. In my own journey recovering from CFS/ME I trained for 3 years to become a Somatic Experiencing Practitioner (SEP), a life changing and transformative education. It is from my training as an SEP that I draw a lot of my understanding of the nervous system in relation to chronic fatigue recovery.
I have a free workshop that you can watch if you want to deepen your understanding in this area. You can sign up here.
A “healthy” nervous system should gently move between states of being more activated and states of being more settled throughout the day. This should be appropriate to environmental cues.
For example, this morning I slipped in the bathroom grabbing my towel after a shower and fell hard on my hip. My body leapt into a state of activation to help me react quickly to the fall but once I was on the floor and I could acknowledge that I was safe, dust myself off and continue with my day, everything settled down again and I moved on.
People who experience chronic illness may often be overly reactive to very small things and / or they get stuck in states of stress with the inability to relax and settle. In other words, their nervous systems are unstable. They react disproportionately to environmental cues and they struggle to unwind and relax. They may become stuck in fight or flight or even in freeze states which perpetuate the imbalances which impact physiology and physical function.
Experiencing a chronic illness is inherently stressful. You are grieving the loss of your health, life, and your identity, as you know it. There are likely devastating financial implications and relationships suffer. You have to adapt to a new way of living your life and cope with the inevitable grief at the same time you are the most under-resourced you have probably ever been.
Which is why we want to cultivate a toolbox from which we can resource ourselves. This means supporting the nervous system to navigate all the changes it is processing.
In my Nurturing Resilience Self Study Program I call these tools, “Stabilising Tools”. These are a specific set of tools, some of which I teach in the Getting To Know Your Nervous System Workshop that helps to create a better sense of grounding, settling and stability in the nervous system.
People who aren’t somatically trained may use the word “calm”. We want to help the system calm down and settle. How you do this is up to you. I am biassed due to my training that Somatic Experiencing is the best way! Yet I also hold space for the fact that there are many different ways for us to heal and the best tools are the ones that work for your body.
Other things that I have found supportive are:
- Yin Yoga
- Restorative Yoga
- Massage
- Craniosacral therapy
- Meditation
- Yoga Nidra
- Time in Nature
- Cuddling Cats
- Brain Retraining (I did the DNRS program)
Things clients find helpful are:
- Reflexology
- Reiki
- EFT
- EMDR
- Humming
For more resources on the nervous system specifically, please refer to the following resources.
Blood Sugar Stability
Blood sugar stability is something that we review with all our clients because, 9 times out of 10, it is not fully optimised.
Many of our clients are prone to low blood sugar. This might mean that when they eat, their glucose is spiking too high and then crashing to a low level 2-3 hours later. This is often experienced as an increase in fatigue and/or loss of function that improves with eating.
Other clients have blood sugar that is generally too high across the day and this can be exacerbating fatigue as energy isn’t getting into the cell.
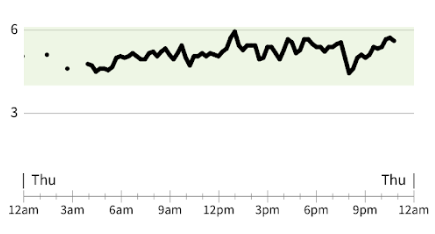
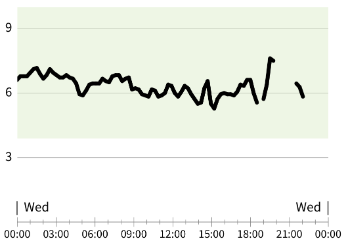
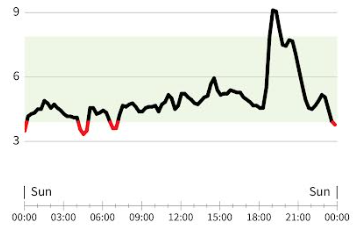
Either way, we want to make dietary changes so that blood sugar remains stable (i.e. not swinging from high to low) and that it also remains within a healthy range across the day (about 4 mmol – 6 mmol/L).
We normally ask clients to use a CGM so that they can track their blood glucose levels. Here are some examples.
How do we optimise blood glucose?
You can read more around this topic here and here or take the Blood Glucose Mini Course.
Generally speaking these are things that work for our Chronic Fatigue Recovery Clients:
- Increase protein intake and aim for 30-40g of protein at each main meal
- Reduce carbohydrate intake, in some cases transition to a low carb or ketogenic diet
- Consume good amounts of fibre, from low carbohydrate sources with a meal
- Avoid sugars, processed carbohydrates and refined grains
It can take time to fully optimise blood glucose depending on your current diet and awareness around food. It is something that may require a high level of discipline and commitment, but definitely worth investing in doing.
Sleep & Circadian Rhythms
Sleep can be a tricky one when it comes to Chronic Fatigue Recovery. Some people need what feels like excessive amounts of sleep to function, while others find sleep elusive, broken and not enough.
For those who need a lot of sleep, the best thing you can do is honour the need to sleep and trust that you will need less as your health improves. I have seen clients who need 2 hour afternoon naps to function, gradually reduce their nap times as time has gone on.
The most important thing is that however much sleep you need, that you have a set routine. This means that you go to bed at the same time each evening and wake at the same time each day.
The next goal, is to view sunlight on your eyes within the first 30 minutes of waking, ideally as follows:
- 3 minutes on a sunny day
- 10 minutes on a partly cloudy day
- 20-30 minutes on a cloudy or rainy day
This should not be through a window or sunglasses. If you wake up before sunrise, expose yourself to bright lights or ideally a 10 000 LUX light and then get outside later in the day.
As your bedtime approaches, have a routine which signals to your body that it is time to relax and unwind.
- Use dim lamps instead of overhead lighting
- Avoid screens or use bluelight blocking glasses
- Don’t engage in activities that you find stressful or activating
- Rather engaged in activities that encourage downregulation of your system e.g. gentle stretches, meditation, yoga nidra
- Use an eye mask or black out curtains in your bedroom (I use this one)
- Time meals appropriately; if you are prone to low blood sugar you may need a snack before bed, others may need to eat 2-3 hours before bed time
- Take sleep support as needed. Some of my favourites are:
- Magnesium glycinate
- L-theanine and Lemon Balm
- Inositol
- Glycine
If this is an area that you struggle with, you can refer to the following links for more details on sleep and circadian rhythms:
What about sleep medications?
Medicated sleep is not as good as non-medicated sleep but medicated sleep is still better than no sleep at all. When the goal is stability, medicated sleep can sometimes help you to feel “rested enough” and therefore able to work on other stabilising factors like your diet, sunlight exposure and nervous system. When these aspects of health are in a good routine you can then discuss with your doctor about weaning off your sleep medication.
Stabilising Energy Output in Chronic Fatigue Recovery
We’ve all been there; you have a little bit more energy one day, you over do it and the next day you get hit by a big “fun tax” bill. Alternatively, you don’t have any more energy than usual but life happens and brings its extra demands and you end up pushing through.
When I first became unwell I was regularly in a cycle of boom and bust, mostly because no one ever sat me down and told me this…
There are no supplements, dietary changes, medications or meditations that will compensate for poor pacing.
Pacing yourself is an essential part of recovering from Chronic Fatigue. Learning to properly pace is how we build stability into our day to day.
What does this actually mean?
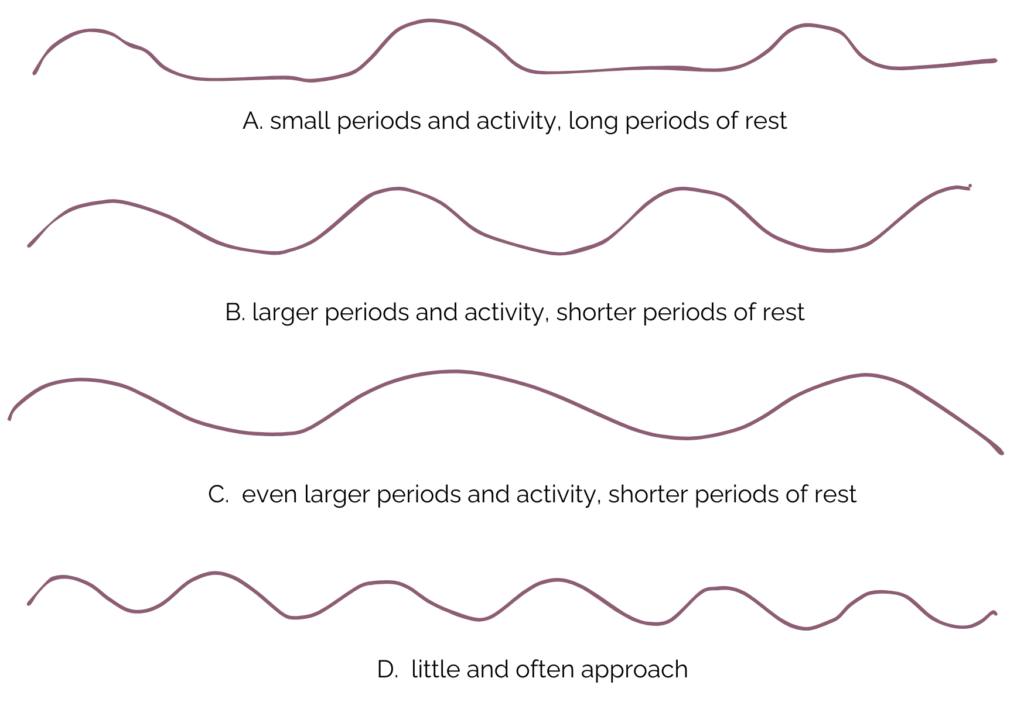
Very simply, each day should be made up of periods of activity and periods of rest. These should be distributed across the day. In other words not one big chunk of activity followed by one big chunk of rest (this is basically just boom and bust).
Depending on where you are in your journey, your periods of activity will probably be quite small and your periods of rest will likely need to be fairly big. However, as time goes on, you may notice that you can do more for longer and that you need less rest between activities to regain your energy. See the diagram below.
Many people are not aware of how much they are doing in a day and not necessarily able to connect how certain things are making them feel. It can be helpful to keep a diary of what you are doing and how you are feeling so that you can notice patterns and trends.
When we ask our clients to do this we always notice the following:
- Continuing for too long before stopping
- Stringing too many activities together
- Not enough time to rest between activities
- Resting is not actual rest
The most helpful thing you can do is start to identify the earliest warning signs that you are starting to fatigue. It could be a subtle increase in pain, brain fog, lethargy, getting irritable, struggling to find words or concentrate. The moment you notice these signs creep in, it is time to rest.
Resting should be proper rest which means that your nervous system should ideally be able to access a parasympathetic state – easier said than done! What this might feel like in your body is that you have a sense of connection to yourself, if you are lying down or seated you feel a sense of weight and heaviness in your body, your body might feel less tense, more open, softer, wider expanded, and there is more breath in your belly.
Being realistic, it might take a while to feel perfectly rested but you want to notice your body shift. A decrease in symptoms isn’t always a sign that you have rested properly, it can be more helpful to track for a sense of feeling more “online” again and ready to do something else.
Things that may be restful include:
- Lying in a dark room without any sensory input
- Lying down and listening to some relaxing music
- Watching a funny TV show
- Doing a meditation or yoga nidra
- Doing a restorative yoga practise
- Sitting in a comfortable chair with your cat
- Sometimes even a short walk outside can feel restful when you have enough capacity
The way pacing is described above is how I learnt to do it, which is based on learning to listen to my body and respond to and honour the feedback. This isn’t always easy and therefore, an alternative option is to use technology such as the Visible App to help you with your pacing.
What about movement or exercise?
When I was ill, all I wanted to do was exercise again. I tried repeatedly to reintroduce exercise into my routine but it just made me worse over the long term and perpetuated cycles of boom and bust. Exercise is a stress on the body. In the right dosage, it can be a positive thing and there is definitely a time and place for it in the Chronic Fatigue Recovery journey. However, when the body is inherently unstable, it can be further destabilising.
Therefore, when it comes to achieving stability, we only want to move (or exercise) at the dosage which does not make us feel worse than we already do. If you are struggling to add exercise or movement to your routine, it might be best to optimise some of the other stabilising factors first, before you work on increasing your movement.
That being said, if there is a level of movement that you do tolerate. You want to do this consistently, ideally at the same time each day, to maintain momentum on which you can build at a later date.
Addressing Infections
There is an area of nuance when it comes to achieving stability. When there is an active infection of some kind, the immune system creates a host of compensatory physiological changes to fight the infection. These changes can be inherently destabilising to our everyday optimal baseline.
When an infection is acute, for example a bout of flu, ideally we would rest well, eat well and allow the immune system to work out the rest.
However, when there is a chronic and ongoing infection, addressing an infection may cause some stability in the short term but may be required to help the body become more stable long term. How do we know what to do?
The answer to this question is likely case specific. However, when working with unstable systems, it is preferable, where possible, to stabilise as much as possible before addressing the infection. However, there are some cases where we may just have to go for it and trust that the individual has enough resilience to bounce back afterwards. This is where it can be helpful to work with a practitioner who can guide and support your case.
Summary and Conclusions
A Chronic Fatigue Recovery Journey is seldom straight forward, it can be complex and nuanced at times. However, many may skip over the basics because they seem too simple to make a difference.
The stabilising principles are not necessarily a fix for all your symptoms but they will help to create strong foundations on which other, more aggressive or disrupted, interventions can be taken e.g. detox or addressing infections.
If you feel lost on your Fatigue Recovery Journey, these principles are a great place to start. If you would like more help in your journey, consider working with one of our practitioners here.