Shownotes
Post-exertional malaise is probably one of the biggest bugbears when it comes to fatigue recovery. Anna shares a general framework for tackling post-exertional malaise as well as her own experience and things that made the biggest difference for her personally.
Useful links:
Website: https://annamarsh.co.uk/
Instagram: https://www.instagram.com/anna_marsh_nutrition/
Fatigue Recovery Quiz: https://app.annamarsh.co.uk/quiz
Post-Exertional Malaise
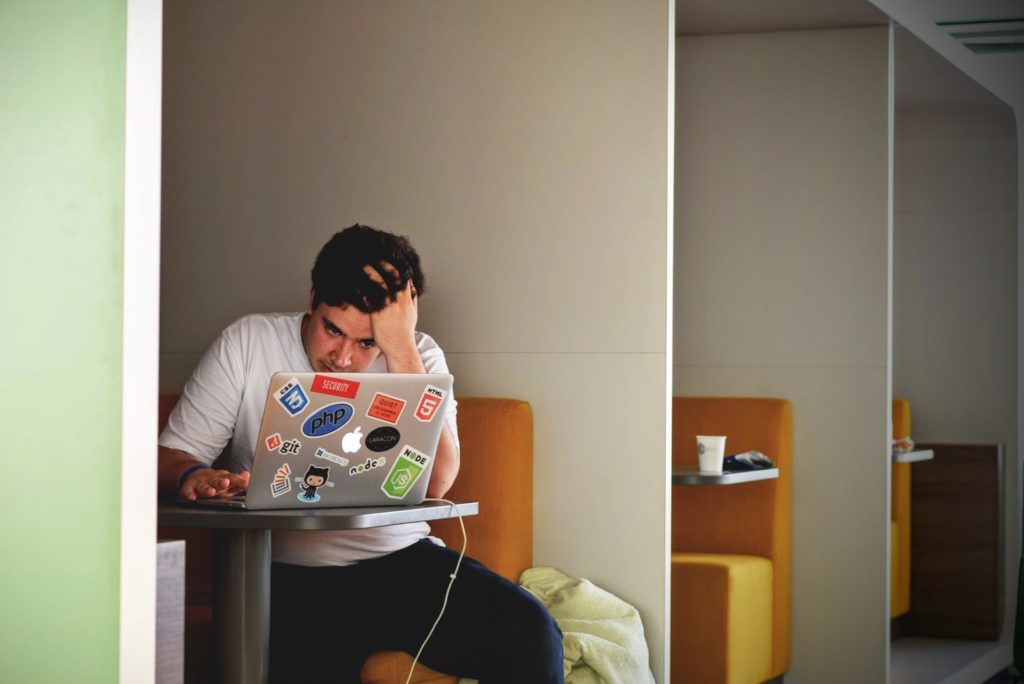
Welcome back to the chronic fatigue and burnout recovery Podcast. Today I’m going to be talking about post-exertional malaise. If you are anything like me or anything like I posted, exertional malaise was one of the biggest bugbears in my fatigue recovery.
It was probably one of the first symptoms to creep in, although I didn’t realize that’s what was happening initially. It was one of those last things I needed to deal with to move forward and gain momentum in my fatigue recovery. I know the frustrations of post-exertional malaise very well, and I’m going to share today some things that you may want to be thinking about if you are as frustrated as I was.
And things that work for me, things that work for clients, and things to play around with my work in general. But before I share all of that with you, I guess the first thing to say is, what is post-exertional malaise? Post-exertional malaise is an increase in symptoms that occurs after exertion, which could sometimes be mental exertion.
For the most part, it is physical exertion or exercise. Usually, it happens between straight off to exercise to 24, even 48 hours after some demand on the body system. I found in my own fatigue recovery that there was definitely a pattern that I would notice.
So if I was going to get any post-exertional malaise after exercise, I might have an hour after I exercise where I would feel on top of the world running on all the fantastic endorphins and then by about almost four hours on the dot after I finished exercising, that’s when it would hit, and I would tend to feel the symptoms increase. For me, a lot of it was experiencing a lot of brain fog, fatigue and maybe some aches and pains. Although it can be different for each person, there will be a bigger cycle.
That was the small four-hour cycle, but the bigger cycle might be like a build-up cycle. If I had been doing a lot of things over, like maybe several days, I knew I could wake up one morning and just need a rest day. That, to a certain extent, was easier to manage because it was a bigger, less intense cycle.
But if I were going to get the sort of crash for hours after exercise, that would probably be the more intense cycle. I tried so many different things and many different approaches to exercise. I was constantly trying and crashing, trying and crashing, trying and crashing.
I wouldn’t recommend it. But eventually, I did get to where I needed to go. Hopefully, what I can share today in this episode can shortcut that process for you so you don’t have to go through those repeated cycles of trying and crashing, trying and crashing.

Exercise was such a big part of my life pre-CFS. I had been exercising, running, swimming, training in gyms, aerobics, spin, yoga, and CrossFit for more for about 20 years when I finally became unwell. It was such a big thing to let go of this ability to have a great workout, and it was always the thing that I wanted to get back the most, and it was the thing that took the longest to get back.
I hope this podcast today will help you get that ability to exercise back sooner rather than later because if you’re anything like me, it’s probably something you are really craving. The first thing to understand about post-exertional malaise is it is kind of like a mini-crash or a crash. You could listen to the previous episode that I did on how to manage crashes, flares and setbacks because it is like a mini crash and mini flare, a mini setback every time you get post-exertional malaise.
It’s important here to understand that inflammatory changes have happened in the body. There are nervous system changes that have happened in the body, which are self-protective intelligence because the body perceives that there is a threat. It might just be the threat is that you’ve produced too much inflammation, too much toxicity, doing whatever physical activity that you just did.
Or it could be that there’s an energy crisis, there’s not enough energy to cope with the activity that’s sending the system into distress. So here, if there’s mitochondrial dysfunction that could be impacting this post-exertional malaise, or it could be that your nervous system is just really not feeling safe enough to exercise yet. Therefore your body is responding with the post-exertional malaise as a self-protective shut down so that you don’t do more than what it can handle right now.
One of the things we want to think about is fatigue recovery, and we need to exercise. Exercise is good across so many levels and beneficial to the recovery process. But we needed to be at the right dose. Suppose you are experiencing post-exertional malaise and you’re trying to exercise. In that case, the first thing is to strip back whatever you’re doing so that you are doing an amount which is tolerable to the body, even if it’s not what you want to be doing.
I think a lot of people focus on walking when they first started to build up their activity and when I first started to build up my walking, I was doing heart rate-controlled walking, keeping my heart rate in a safe zone, and that was enough. But then, over time, I could maybe add in a little bit of swimming, and I worked out if I did a teeny tiny bit of swimming. Then I bobbed in the water for a bit, did a teeny tiny bit of swimming, and then bobbed in the water for a bit.
I could do quite a bit across about 20 minutes or so, but it was very slow going. The frustration is that if you love to exercise, and you’re used to being able to do loads of exercise, to do very, very small amounts is disheartening. But you need to remember that what you’re doing is you’re conditioning your body to get used to exercising so that the exercise is less threatening to your system.
You’re producing less inflammation as a consequence of doing the exercise because your body is used to it. So you want to find the minimum tolerable dose and then build up from there. The other thing you can do is buffer your exercise practices with restorative practices.
What that might mean is if you go out for a walk, and then you come back from your walk, maybe that’s when you do a little bit of nervous system self-care of, visualization and meditation. Sometimes I would just come home and put my legs up the wall to slow down my heart rate to get blood flow back to the brain, and I would do 15 or 20 minutes with my legs up the wall. When I was doing my walking, I would walk along the beach to a certain point, and then I would sit on a rock, I would do some breathing exercises, a little bit of visualization and a little bit of nervous system work, and then I would walk back and then would do the same when I got home.

When I eventually started doing weight and resistance training again, I would finish my resistance training with about 15 or 20 minutes of yin yoga to really calm my body down. Even still, once I finish a workout, now I’m exercising how I used to, I’ll still take a little bit of time at the end of the workout to do some stretching to bring my heart rate down to recenter my nervous system, so that’s an ongoing practice for me. The next thing you can start to think about is supporting inflammation in the body.
To a certain extent, this is what you’re probably doing as part of your healing journey anyway. In the broader context, should I say it’s making sure that your diet is optimized, you’re consuming lots of anti-inflammatory foods, you’ve got very stable blood sugar, and maybe you’re doing some fasting? Then on top of that, we can think about adding in some anti-inflammatory support around exercise.
The type of support I like specifically from a supplement perspective is glutathione. Glutathione is one of the master antioxidants in the body. So if I’ve done even now if I do a workout, which is quite strenuous, I might have some glutathione in the evening before I go to bed to support my recovery overnight.
The other thing that I like to do is add curcumin. I liked the Nutri advanced curcumin and I take 1000 milligrams, as soon as I finish a workout, so that’s two tablets after the workout, to bring down the inflammatory load from the workout. There is also research to suggest in long COVID that having 1.5 grams, so 1500 milligrams of L-citrulline and 500 milligrams of vitamin C daily can help with post-exertional malaise and exercise tolerance.
And generally speaking, I also like to add some sports nutrition to my workout. I’ll usually take creatine, branched-chain amino acids and electrolytes if I go for a long hike or even a long walk, or if I am doing something a little more vigorous, like a bit of swimming or weights workout, I would take those supplements. You don’t necessarily have to wait until you’re exercising like an athlete to support your body as an athlete would.
I always say that recovering from chronic fatigue syndrome is like being a professional athlete. Because athletes have to, you know, challenge their body, they do their training for the day, and then the rest of the day is about supporting recovery. It’s the same for chronic fatigue, we spend some of our days challenging the body so that we expand the capacity of the nervous system and the different body systems, and then we spend the rest of the day doing as much as possible so that we can restore, repair, and grow stronger over time.
A big thing you may also want to think about is what is going on in your gut. I’ve done a whole podcast on digestive health, so I won’t go into gut health in detail here in this podcast today but remember that inflammation in the gut can commonly be associated with inflammation in the rest of the body. If there’s an overgrowth of bacteria that produce toxins in your gut when you exercise, your gut barriers become a little bit leakier.
Then those toxins will pass through into the bloodstream, which will contribute to the body’s toxic load, in addition to toxic byproducts that may be getting stirred up from exercise. And remember that if any inflammation is generated through exercising, your lymphatic system and your detoxification pathways will have to process those inflammatory molecules as well. It’s a lot.
If the gut isn’t working very well, it’s an extra load that can contribute to this post-exertional malaise. If you want to do more exercise and you have digestive symptoms, remember that you don’t always have to have digestive symptoms. Still, if you do, you may want to consider addressing your digestive health before you think about expanding your exercise capacity.
A big one I wanted to mention was mould. This was possibly one of the biggest blind spots in my own chronic fatigue recovery journey. Mould had never really crossed my mind until I had been unwell for about three years, which is a long time.
I was getting so frustrated because of the post-exertional malaise I was experiencing. I would make a little progress and exercise capacity and then feel like I’d go back to square one again. I was so desperate to exercise.
I was at the point where I could hike, and I could walk, you know, provided it wasn’t too strenuous or terrain. I could walk for three hours, but the moment I tried to do anything more intensive than walking or anything resistance-based, I would go into this post-exertional malaise inflammatory state. I could not tolerate it.
Eventually, I decided to test myself for mould. The test came back positive. I started a detoxification and drainage support plan, and within a month of starting that, I could build up my resistance training.
And then, as I continued to detox more and support my body more, I was able to do more and more and more and more, and it was the final kind of nail in the coffin of three years and the making that enabled me to get my exercise back to where I wanted it to be. It was really important to me that I could resistance train because there are so many health benefits to having adequate muscle mass. Adequate muscle mass is important for metabolic health and is anti-inflammatory.
The more muscle mass you have, you’re likely to have better the quality and quantity of mitochondria, which means you have a more resilient nervous system. It supports just posture, and it’s anti-ageing. Resistance training is really important for women for their bone health.
There are so many reasons why I wanted to resistance train and it wasn’t until I addressed the mould that I was able to do that. I looked into it a little bit more at the time and one of the mechanisms is that mould increases something called vascular endothelial growth factor or VEGF. Essentially, this blocks the capillaries in the body, which ultimately prevents good blood flow and oxygenation of your cells.
There’s a link here with the increase in VEGF in long COVID. That’s worth noting. This is how mould can impact exercise capacity and cause post-exertional malaise. Still, there are a few other mechanisms if you have a lot of mycotoxins in your body. You’re exercising, that’s potentially moving them around the body, mobilizing them, and adding to the toxic load that may be coming in from tissue breakdown when you’re exercising.
We’ve got the poor oxygenation and poor circulation, we’ve got the toxins in the body, which are getting mobilized, we’ve got the toxins from exercise, and we’ve also got the inflammation that has been produced by tissue breakdown. Your body has to deal with all of that. Suppose you can’t deal with all that will cause foggy brain, fatigue, and inflammation until everything can settle down and find homeostasis again.
I don’t think it matters to eliminate the toxins, whether it’s mould, mycotoxins or other mycotoxins, but supporting the liver, detoxification, and reducing the body’s toxic load as a whole, is another thing that you can do to support post-exertional malaise. This is where in some cases, a sauna can be really helpful. The sauna is always a bit delicate because some people may or may not be able to tolerate the sauna.
I have some clients who can’t even tolerate a hot bath so the idea of going into a hot sauna is it’s just a no-go. But if you can tolerate a sauna, whether five minutes, 10 minutes, 15 or 30 minutes, it can be beneficial post workout for muscle growth and hypertrophy gains. But I found it was great for muscle recovery.
If I was feeling a little bit foggy-brained after a workout, I could have a sauna, which will nip in the bed. So really, great for detoxification. You can support your body around the sauna with antioxidants, glutathione, and binders, but that’s another story for another day.
But sauna can be complementary to reduce post-exertional malaise if tolerated. I probably was in the worst state with mould illness, and I didn’t know I had mould illness. I remember just trying to sauna would make me have post-exertional malaise.
We need to tread cautiously, but if you can tolerate it, it’s a great thing to add in. Then another thing to consider is histamine. This is where there is a little bit of overlap with mould as well. Exercise can increase histamine production.
If you are already somebody who has mast cell activation syndrome MCAS. Suppose you suspect that you are quite a histamine intolerant. In that case, exercise could push the histamine levels in your body over the edge, which could be responsible for some of your symptoms.
Mould is something that can be a histamine trigger. Still, there can be other things too, like parasites, for example, dysbiosis in the gut, other infections, and foods can send histamine levels up, so we want to consider here in this case, if you do think that maybe there’s a histamine load on the body, which is getting pushed over the threshold with exercise, we need to circle back and deal with the histamine issue, which means that we want to remove any possible histamine triggers, and then support the body as much as possible to process histamine. That could be looking at molybdenum deficiency or using things like quercetin, cumin, and antioxidants to reduce the histamine to improve the breakdown.
Again, I don’t want to go into histamine’s full ins and outs in this podcast because it’s potentially a full podcast. Still, if there are any female hormone imbalances, particularly high estrogen levels, that can influence histamine production, which might mean exercise tolerance varies at different parts of the menstrual cycle. You could plan maybe your exercise around your menstrual cycle, but that’s more of a band-aid approach.
We want to stabilize the hormone and histamine so you can train them across any part of your cycle. Then just a couple of other things. Oxygenation of the body is really important. I explained how in mould, we get that increase in the VEGF, and that decreases oxygenation and causes the post-exertional malaise. Still, anything that decreases oxygenation could be contributing to post-exertional malaise.
Here, we want to be nasal breathing with exercise. You never want to be mouth breathing if you have a chronic illness. Athletes pushing themselves to very high intensity may, on occasion, mouth-breathe.
Still, for the most part, if you’re a regular human exercising at moderate intensity, it’s nasal breathing. Then we also want to think about supporting the circulatory system and supporting the vascular system. Here we have a compound which is called nitric oxide, which is a vessel dilator.
It dilates the blood vessels, which means we get more blood flow and better oxygen transport. Here things like beetroot, for example, is a vessel dilator. The L-citrulline I mentioned previously, shown to be beneficial in long COVID can also be a vessel dilator.
Dark chocolate, berries, garlic, green tea, herbal supplements like ginkgo Biloba, or go-to cola can also be beneficial in supporting oxygenation. You can go back and listen to the oxygenation episode of this podcast, where I talk a little bit more about creating healthy red blood cells, how to test for that, and the nutrients involved. The final one is just herbal adaptogens.

These are often given to the adrenal glands, but they may also have benefits in supporting the immune system. Remember that the inflammatory load created by the immune system could be responsible for the post-exertional malaise. If we can take herbs that modulate the immune system, reduce inflammation, support oxygenation, or many other processes in the body, this could be helpful.
Things like quadriceps, Rhodiola, Siberian Ginseng, or Schisandra, any of those could potentially be beneficial. In my fatigue recovery, I would do quadriceps sometimes, usually put it in my coffee to make like a little mushroom coffee or decaf coffee that I will buy from my mushrooms, which I’ll put a link for into the show notes for you. That’s a lot to think about regarding the post-exertional malaise.
I’ll recap on everything discussed so far. We want to make sure we’re starting to find that optimal workload. How much can we tolerate, however big or small, buffering that workload with restorative practices, so the nervous system is winding down and being restabilized after exercise?
Then we add anti-inflammatory support, if appropriate. We want those baseline anti-inflammatory practices in there. So diet, blood sugar, gut health, and anti-inflammatory supplements post workout if required.
If there are any digestive issues, we want to address that; if there are any lingering immune triggers, like mould or maybe some other type of infection, that’s a priority to be addressed before we consider expanding exercise capacity. If there are histamine issues, we want to address that. We want to think about how to oxygenate the body as best as possible.
We can use a sauna for recovery or detoxification and, finally, maybe consider some herbal adaptogens as the cherry on top. That brings me to the end of today’s episode. If you have enjoyed the episode, please make sure you’ve subscribed and shared it with anybody you think it would be beneficial. And please leave a five-star review on iTunes, as those reviews help other people find the information too. I will see you in the next episode.